Good spot @DerekGriffin86. A few years ago I spent weeks searching through the lit on normal abnormalities. It's always good to have this sort of data to hand to put things into context. See below for a thread on this article. https://link.springer.com/article/10.1007/s00256-020-03394-z#Tab5
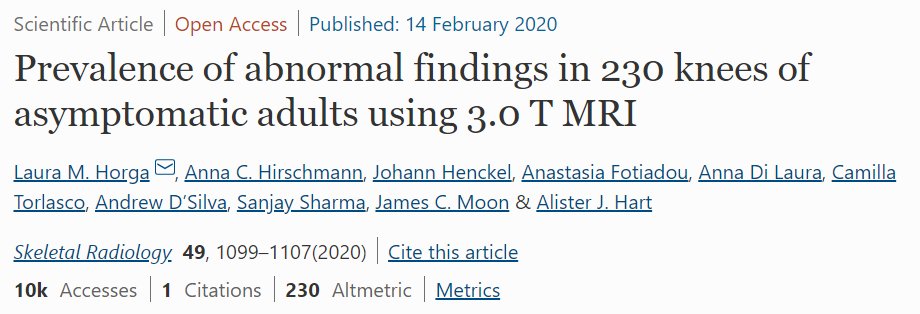
Percentage Prev of meniscal lesions in 115 asymptomatic people (230 knees).
51 males, 64 females; median age: 44 years, range 25–73 years.
Most likely findings seem to be medial aspect, usually posterior horn, and with Extrusion and Degeneration being the most common labels.
51 males, 64 females; median age: 44 years, range 25–73 years.
Most likely findings seem to be medial aspect, usually posterior horn, and with Extrusion and Degeneration being the most common labels.
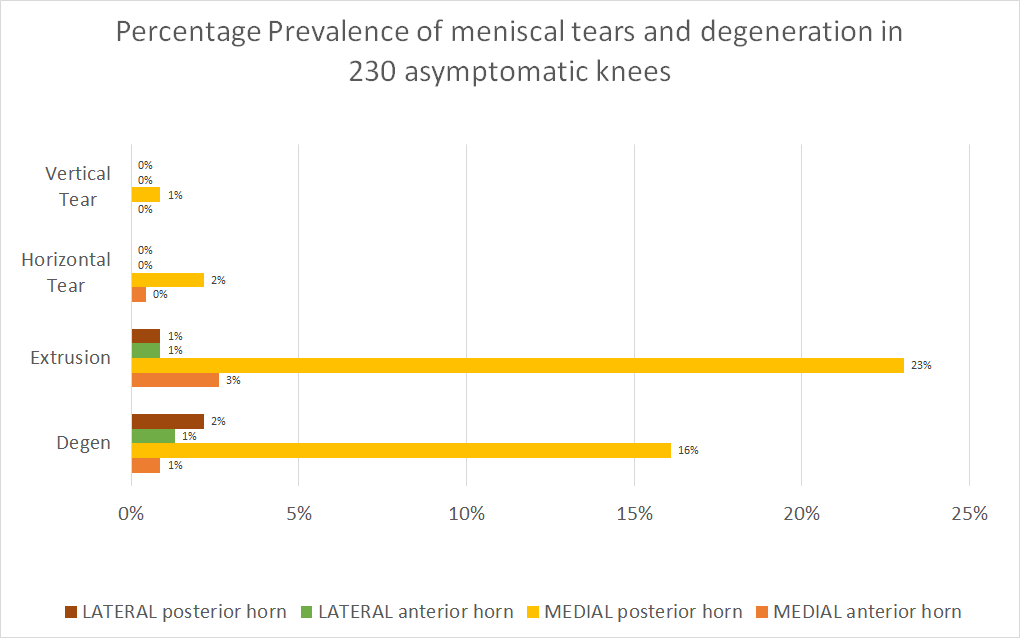
Prevalence of abnormalities of the articular cartilage (same pop). Left graph includes "Any grade" (therefore larger number) and (Grade 0). I have removed in the right graph, but the left one is important for transparency of findings.
The interesting finding here for me is PFJ.
The interesting finding here for me is PFJ.
With a 1/4 of people having Grade 4 changes visible on MRI (again asymptomatic). This is important to consider when imaging that there are likely to be more visible findings here than in the rest of the knee joint (cartilage wise).
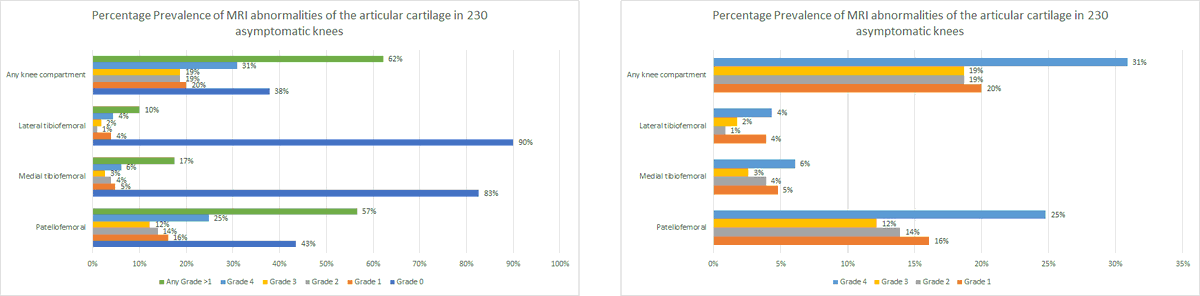
I've done the same for the graphs on Bone Marrow changes. Again suggesting higher prevalence in the PFJ than the rest of the knee joint.
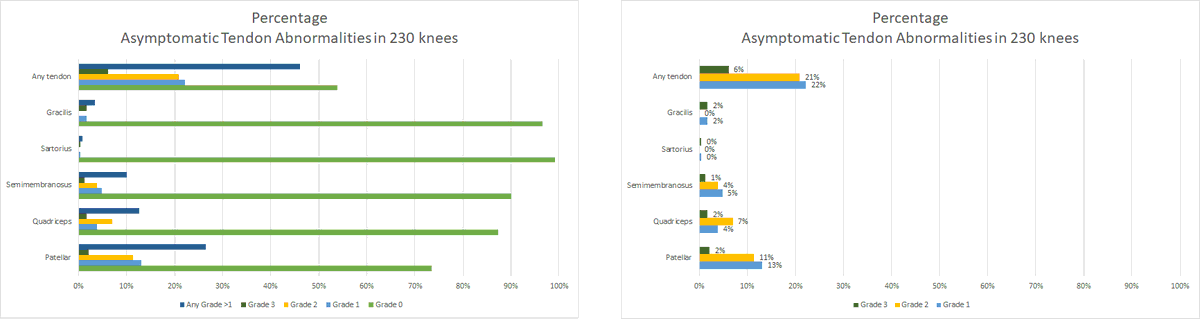
Same again for Tendon abnormalities. Important to note here that Grade 0 is a high number, suggesting few abnormalities in asymptomatic people. The exception being the patella tendon.
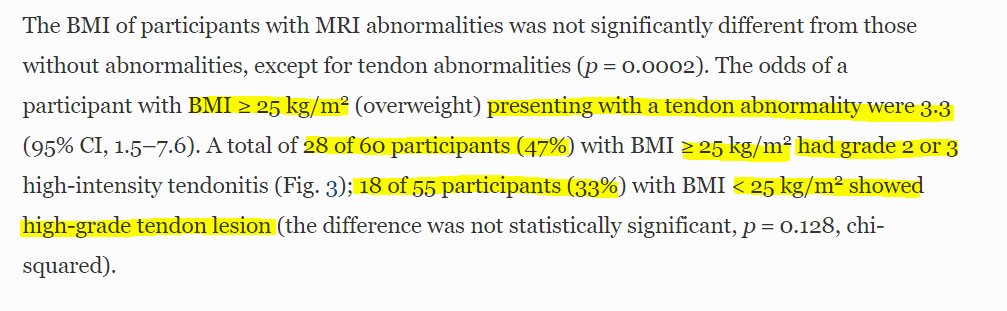
The authors note BMI did not seem to influence general findings here, with the exception of tendons. (This cohort were considered sedentary)
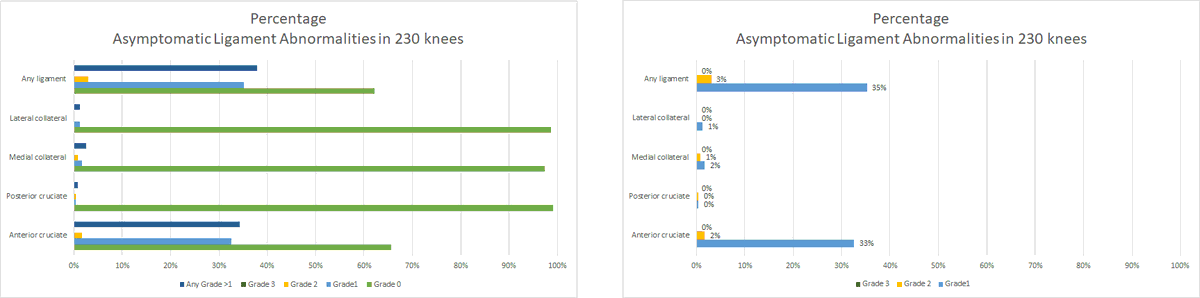
Again high levels of grade 0 here. The surprising one for me was the relatively high number of ACL abnormalities seen - not my particular area of research so it may not be as surprising for some like @richnorris00.
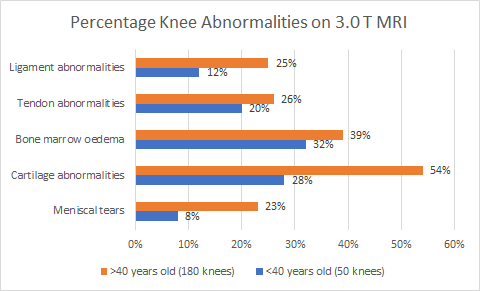
The final bit of stratification was on those <40 years old, and those >40. There was an association with higher findings in those who were older, with more than half having cartilage findings, a quarter with meniscal tears, and almost half with bone marrow oedema.
This paper should not serve to vilify MRI in those with knee pain. My takeaways are:
* As always, context and clinical reasoning is key.
* Use this to frame likely findings prior to referring and when the results return.
* Careful how to deliver your feedback to people....
* As always, context and clinical reasoning is key.
* Use this to frame likely findings prior to referring and when the results return.
* Careful how to deliver your feedback to people....
.... telling someone it's normal w/out context building pre referral will likely lead to "well I know there is something wrong with my knee."
Absence/presence of findings do not tell us something is/isnt wrong, rather, there may/may not be a surgical target if things corelate.
Absence/presence of findings do not tell us something is/isnt wrong, rather, there may/may not be a surgical target if things corelate.

 Read on Twitter
Read on Twitter