B.C. health officials provide #COVID19 update #bcpoli https://www.pscp.tv/w/cnxoIzEyOTUwMTJ8MU1ueG5sWU1wcEJHT1elUDdoOMcin1L2p-HgD3oAOO1fdJ-3s3yv5YVF0wRt
New cases = 1,130
Tues - Wed = 536
Wed - Thur = 594
Total # of cases = 20,368
Tues - Wed = 536
Wed - Thur = 594
Total # of cases = 20,368
Vancouver Coastal Health = 249
Fraser Health = 808
Island Health = 16
Interior Health = 34
Northern Health = 23
Residents outside of Canada (visitors + TFWs) = 0
Fraser Health = 808
Island Health = 16
Interior Health = 34
Northern Health = 23
Residents outside of Canada (visitors + TFWs) = 0
Active cases = 5793
Hospitalization = 155
Critical care or ICU = 44
New deaths = 4 (3 in LTC, another elder in the community)
Total number dead = 288
Close contacts w/active daily follow up = 11,091
Number of people recovered = 14,089
Hospitalization = 155
Critical care or ICU = 44
New deaths = 4 (3 in LTC, another elder in the community)
Total number dead = 288
Close contacts w/active daily follow up = 11,091
Number of people recovered = 14,089
Outbreaks
New = 6 (Nanaimo Regional Hospital, and others); 3 outbreaks declared over
Active outbreaks = 41 (35 in LTC, 6 in acute care); 1,331 people affected
New = 6 (Nanaimo Regional Hospital, and others); 3 outbreaks declared over
Active outbreaks = 41 (35 in LTC, 6 in acute care); 1,331 people affected
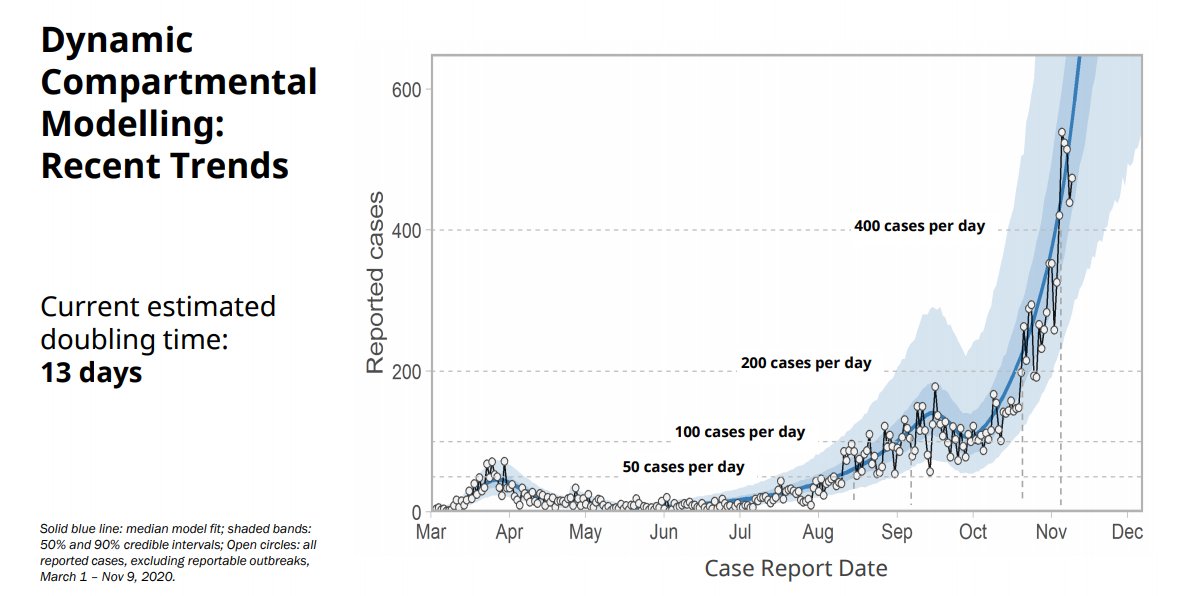
Dr. Bonnie Henry is now providing a modelling update.
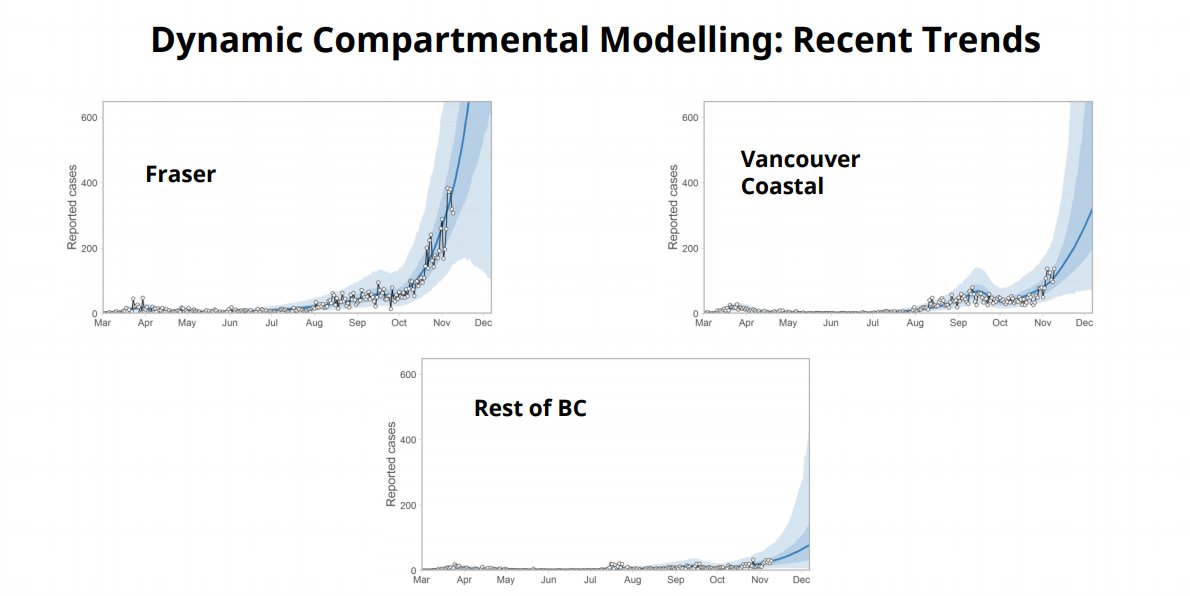
The pandemic has affected every area of the province. The intensity of transmission has been concentrated, particularly in the last few weeks, in the Vancouver and Fraser Health regions.
The pandemic has affected every area of the province. The intensity of transmission has been concentrated, particularly in the last few weeks, in the Vancouver and Fraser Health regions.
B.C. has had the highest number of new cases yet this week (3,121). Median age has come down, stayed within the low to mid-thirties.
Early on, hospitalizations were 20 per cent; now they are 6 per cent.
Early on, hospitalizations were 20 per cent; now they are 6 per cent.
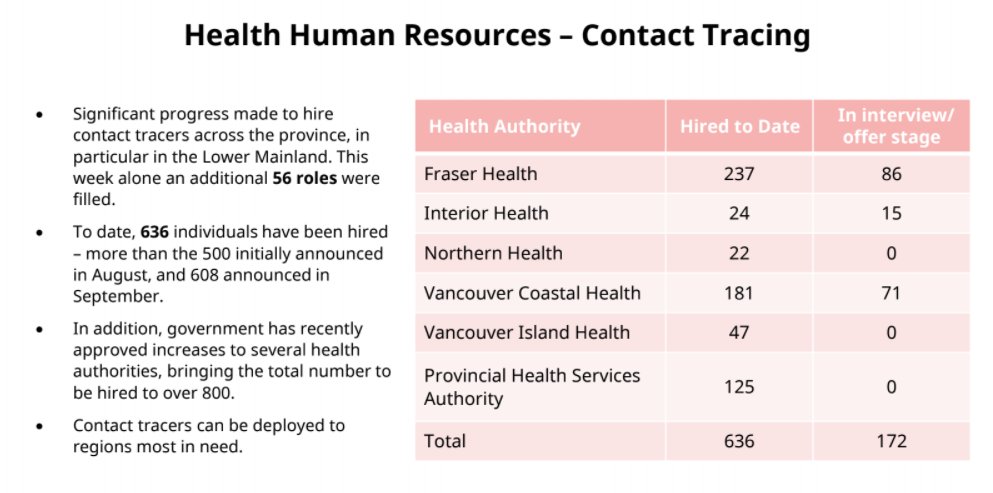
Dr. Henry: The vast majority of cases we can still link to a local cluster. With our rapid increase in numbers, this has been put in jeopardy. The ability to find everybody … has been stretched to the max, and we have fallen a little bit behind.
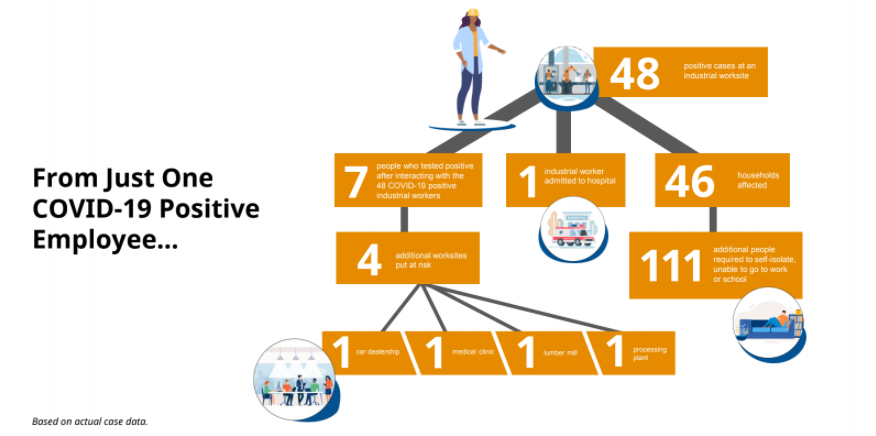
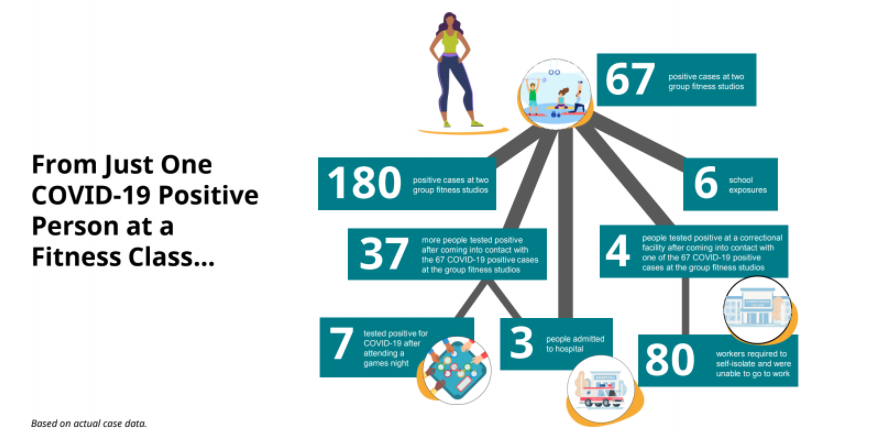
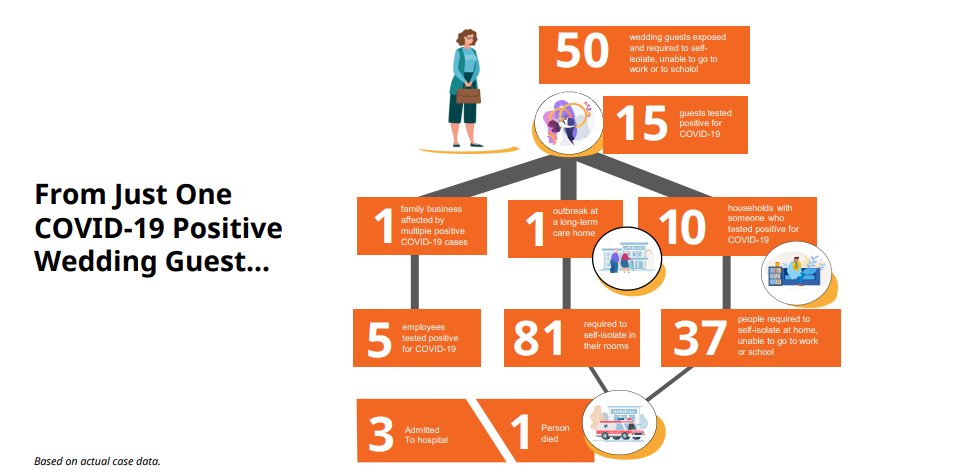
In the summer, younger people were more likely to be infected; that decreased a bit, but recently, young people are again driving infection in the province (work and social gatherings), which is spilling over into other age groups including long-term care homes.
Dr. Henry: Primary source of transmission is households and community interactions; having people over to our house, holding family gatherings and celebrations. Other examples: congregating before gym, at hockey game. Very few transmission events in schools or daycares.
Henry: Health care workers ⇒ rate of transmission has gone down; less than 10 per cent of all cases involve health care workers; majority of health care workers affected are nurses and care aides.
Dr. Henry: It's not that businesses are bad or doing the wrong thing. Indoor settings are riskier than outdoor settings. Ventilation issues indoors; music is really loud, someone is talking very loud; this can very rapidly spread the virus.
Dr. Henry: The safety plans we thought were adequate are not adequate now. There are things we could get away with in the summer; virus doesn’t spread when it is warmer, etc. When we’re moving to cough and flu season, virus finds it easier to spread.
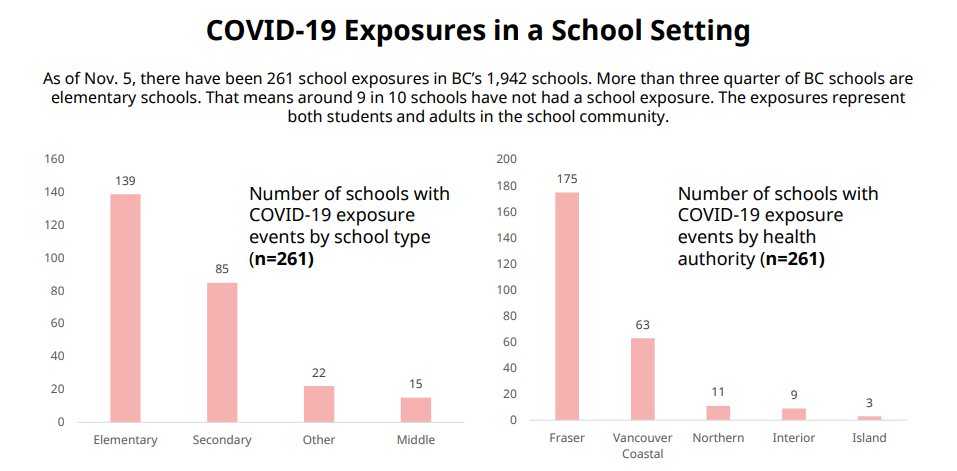
Dr. Henry now providing an update on testing in schools.
School cases ⇒ we know that there have been a lot of coughs, runny noses, lots of testing. ⅔ of the tests are done via spit and gargle test. Vast majority of those tested are not carrying COVID.
School cases ⇒ we know that there have been a lot of coughs, runny noses, lots of testing. ⅔ of the tests are done via spit and gargle test. Vast majority of those tested are not carrying COVID.
Dr. Henry: Very few transmissions in schools; there have been 261 school exposures in B.C.’s 1,942 schools.
1 outbreak.
9/10 schools have not had a school exposure event; this has been a focus because we know how important it is for children to be in the school environment.
1 outbreak.
9/10 schools have not had a school exposure event; this has been a focus because we know how important it is for children to be in the school environment.
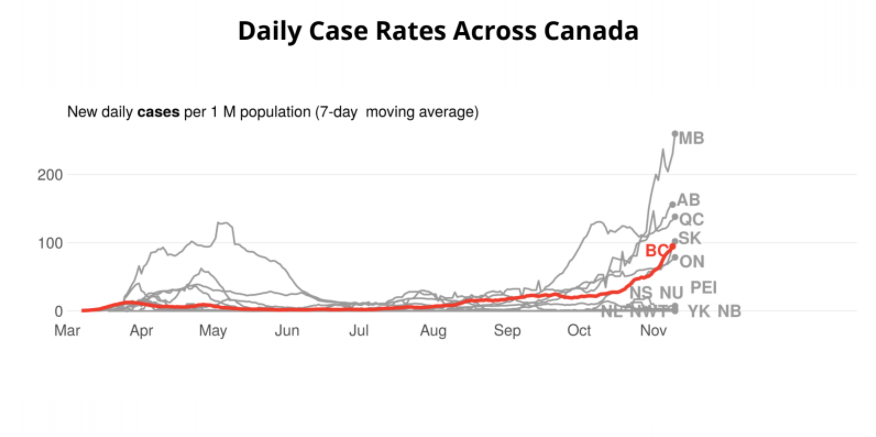
Dr. Henry: Case rates have been increasing; we’ve surpassed Ontario in the past couple of days. That is concerning.
The increase is stretching our ability to cope; we’re not alone in this. We are all learning and trying to manage what is happening in our jurisdictions.
The increase is stretching our ability to cope; we’re not alone in this. We are all learning and trying to manage what is happening in our jurisdictions.
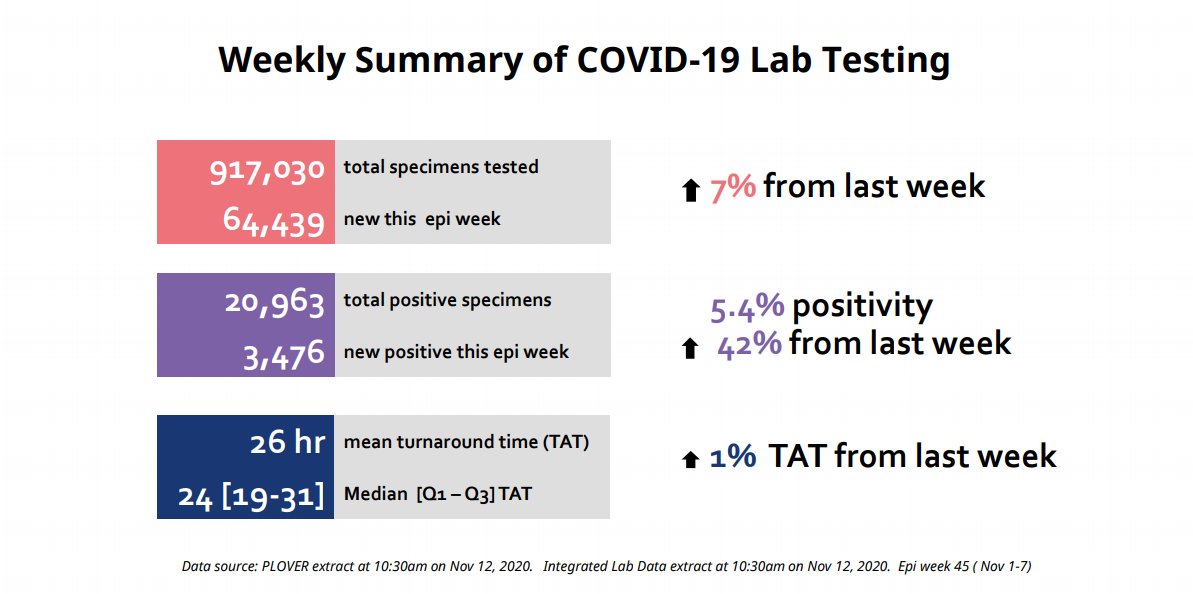
Dr. Henry: The positivity rate has gone up. We’re testing more people, we’re focusing on people with symptoms; 5.4%
As we start to see more influenza, we’re going to have to manage our testing capacity.
As we start to see more influenza, we’re going to have to manage our testing capacity.
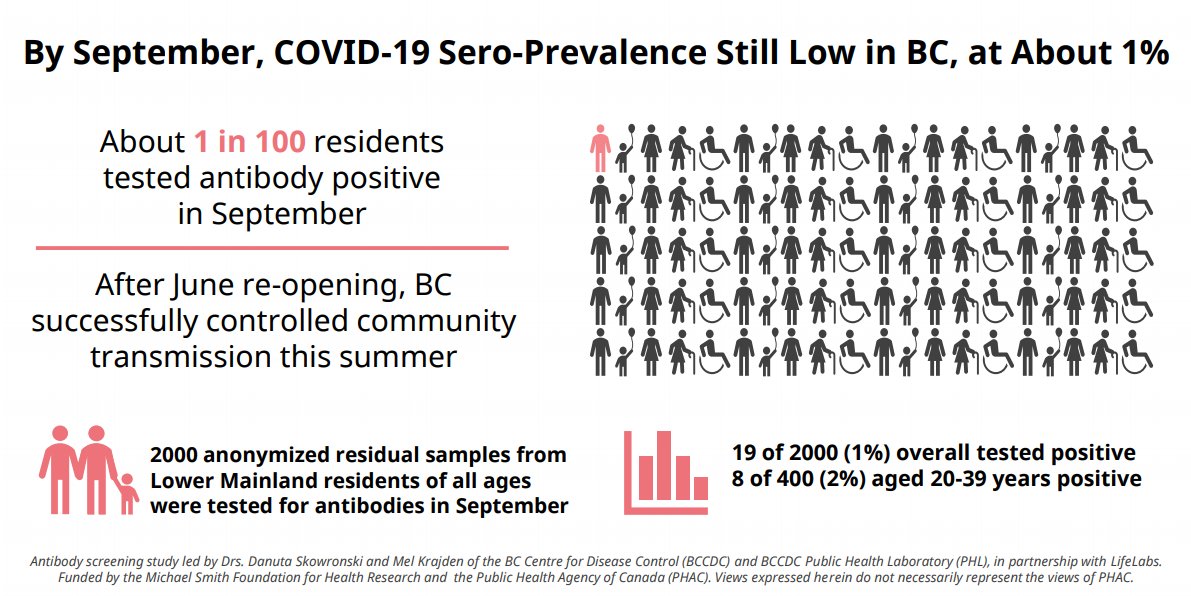
Dr. Henry: Sero-prevalence ⇒ looks at how many people have anti-bodies for COVID-19. It’s about 1 per cent in B.C. So we’ve done a good job in keeping it low. We’re now in a second phase.
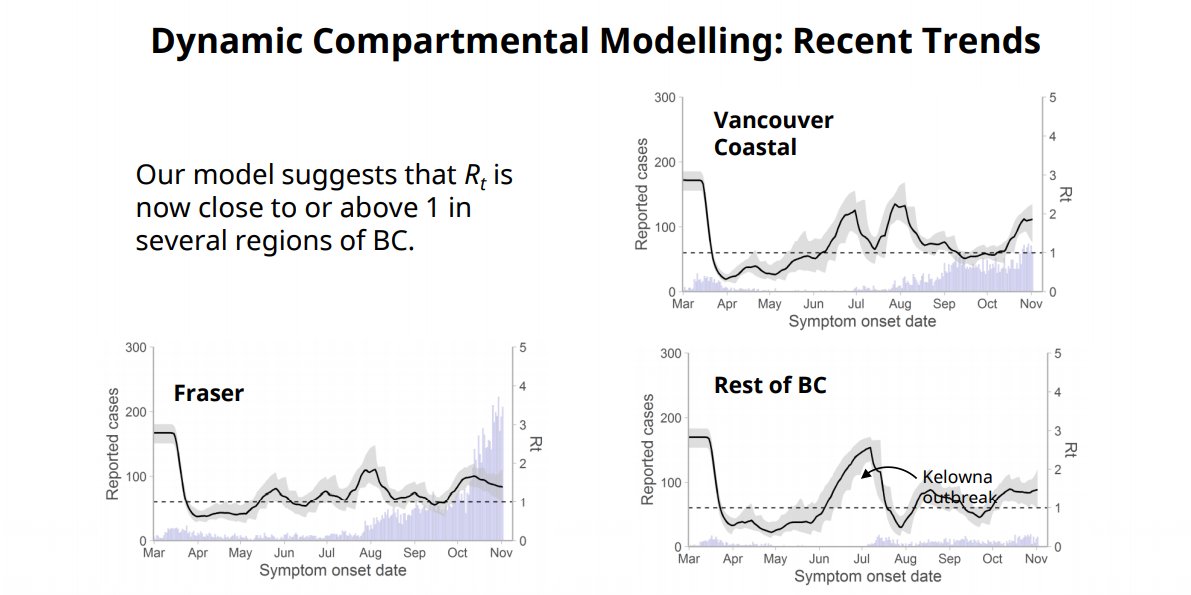
Dr. Henry: VCH + Fraser Health ⇒ that’s the highest number of cases; our modelling shows us that we are above reproductive rate.
We need to take measures to reduce probability we will spread the virus.
We need to take measures to reduce probability we will spread the virus.
Dr. Henry: Our social interactions spread the virus. We’re seeing increase in hospitals, more people in LTC being affected.
Virus transmits much more easily inside; we need to get back to the levels where contact tracing can control the spread.
Virus transmits much more easily inside; we need to get back to the levels where contact tracing can control the spread.
Health Minister Adrian Dix: Contact tracing update ⇒ 636 individuals hired; 172 in offer and interview stage. Shifted some resources to Fraser Health authority to meet demand there.
Dr. Henry: What we’re seeing today and yesterday, numbers that make me slightly anxious, reflects exposures a week ago. I don’t expect to see changes until next week, Monday and Tuesday.
Should BC-ers prepare for extended restrictions?
Dr. Henry: We are going to watch the impact. A possibility we will have to do more or different things. Or possibility we go back. Our hope is to do a circuit break where we can manage again.
Dr. Henry: We are going to watch the impact. A possibility we will have to do more or different things. Or possibility we go back. Our hope is to do a circuit break where we can manage again.

 Read on Twitter
Read on Twitter