1/
A #tweetorial on carotid near-occlusion:
A right-handed patient presents with 3 transient recent events: left BRAO, expressive aphasia, and right hand weakness. Imaging revealed a left carotid near-occlusion, which is defined as having ≥2 of the following 4 criteria:
A #tweetorial on carotid near-occlusion:
A right-handed patient presents with 3 transient recent events: left BRAO, expressive aphasia, and right hand weakness. Imaging revealed a left carotid near-occlusion, which is defined as having ≥2 of the following 4 criteria:
2/
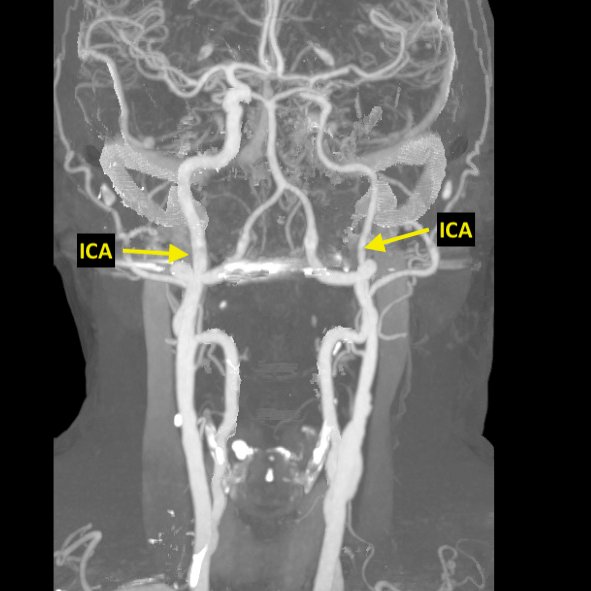
Criteria 1: Reduction of the distal ipsilateral ICA diameter in comparison to the contralateral ICA (as seen on their CTA)
Criteria 1: Reduction of the distal ipsilateral ICA diameter in comparison to the contralateral ICA (as seen on their CTA)
3/
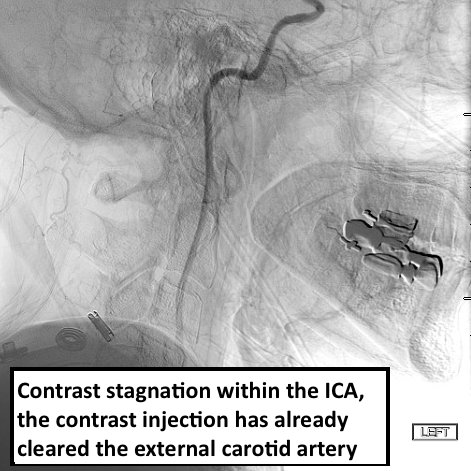
Criteria 2: Delayed contrast filling of the ipsilateral internal carotid artery (ICA) compared to external carotid artery (ECA).
In this carotid injection, stagnant contrast remains within the patient's ICA even after clearing the ECA circulation.
Criteria 2: Delayed contrast filling of the ipsilateral internal carotid artery (ICA) compared to external carotid artery (ECA).
In this carotid injection, stagnant contrast remains within the patient's ICA even after clearing the ECA circulation.
4/
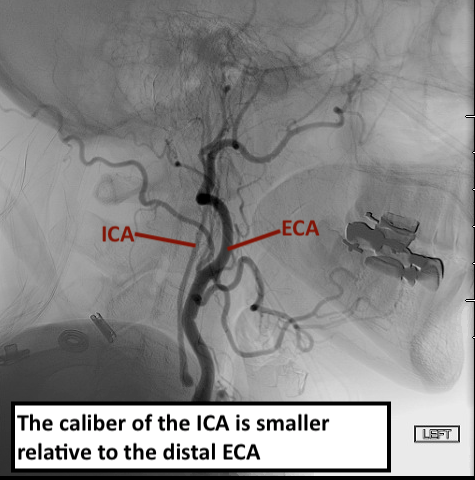
Criteria 3: Reduction in the ipsilateral distal ICA diameter compared with the ECA diameter beyond the facial and occipital artery origins.
Criteria 3: Reduction in the ipsilateral distal ICA diameter compared with the ECA diameter beyond the facial and occipital artery origins.
5/
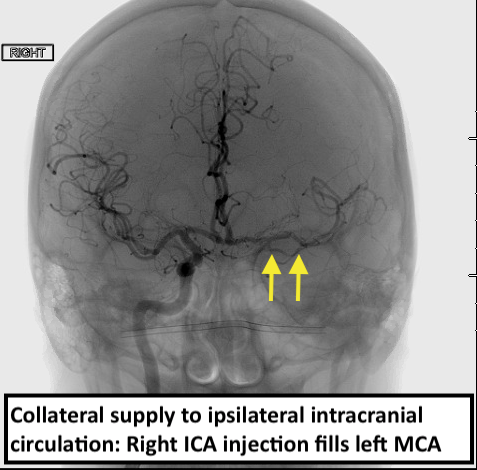
Criteria 4: Evidence of collateral supply to the distal intracranial vessels.
This is seen on the right ICA injection which also fills the left middle cerebral artery
Criteria 4: Evidence of collateral supply to the distal intracranial vessels.
This is seen on the right ICA injection which also fills the left middle cerebral artery
6/
This patient meets all 4 criteria for the diagnosis of carotid near-occlusion. This is important bc: 1) NASCET-defined stenosis measurements using distal ICA diameter are unreliable, 2) this vessel could appear occluded on MRA or ultrasound, and most importantly...
This patient meets all 4 criteria for the diagnosis of carotid near-occlusion. This is important bc: 1) NASCET-defined stenosis measurements using distal ICA diameter are unreliable, 2) this vessel could appear occluded on MRA or ultrasound, and most importantly...
7/
3) although the risk of recurrent stroke and the benefit of carotid revascularization increase with increasing degree of stenosis, paradoxically this relationship is not maintained in carotid near-occlusion physiology.
3) although the risk of recurrent stroke and the benefit of carotid revascularization increase with increasing degree of stenosis, paradoxically this relationship is not maintained in carotid near-occlusion physiology.
8/
In NASCET and ECST, one in five patients with severe carotid stenosis met criteria for carotid near-occlusion. After pooling the patients, the benefit of CEA in carotid near-occlusion was not statistically significant.
http://www.ajnr.org/content/26/8/2086.long
In NASCET and ECST, one in five patients with severe carotid stenosis met criteria for carotid near-occlusion. After pooling the patients, the benefit of CEA in carotid near-occlusion was not statistically significant.
http://www.ajnr.org/content/26/8/2086.long
9/
On the other hand, recent non-randomized publications have suggested a higher rate of ipsilateral ischemic stroke in symptomatic near-occlusion than observed in prior trials. This could be explained by delayed enrollment in previous studies. https://link.springer.com/article/10.1007/s00415-019-09605-5
On the other hand, recent non-randomized publications have suggested a higher rate of ipsilateral ischemic stroke in symptomatic near-occlusion than observed in prior trials. This could be explained by delayed enrollment in previous studies. https://link.springer.com/article/10.1007/s00415-019-09605-5
10/
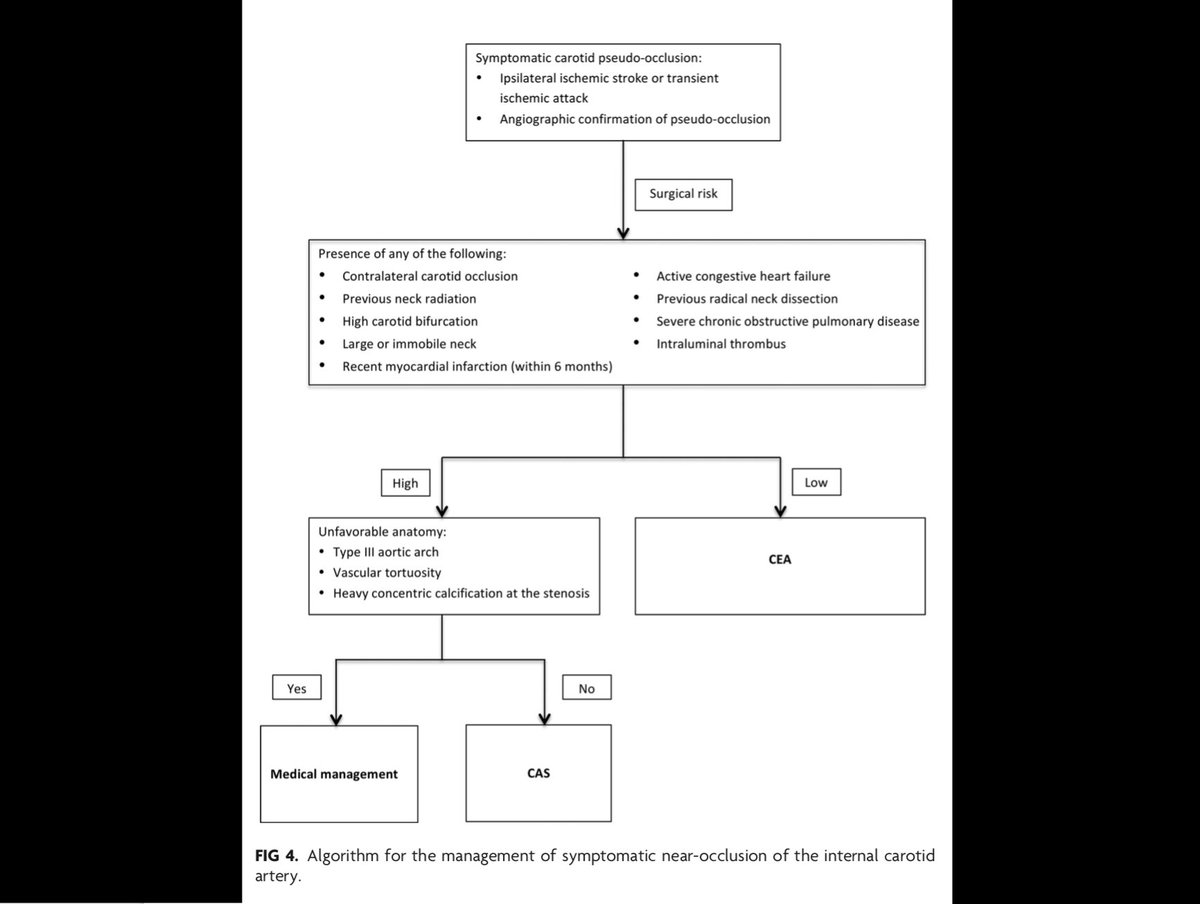
So how should this patient be managed?
The risk of recurrent ischemic events is low, however, perioperative risk is also low. It is reasonable to pursue revascularization given an overall trend towards benefit if no contraindications are present. A proposed algorithm:
So how should this patient be managed?
The risk of recurrent ischemic events is low, however, perioperative risk is also low. It is reasonable to pursue revascularization given an overall trend towards benefit if no contraindications are present. A proposed algorithm:
11/
Furthermore, her clinical course suggests high risk of recurrence, although her medical therapy was not previously optimized. Our own data suggests equivalence between endartectomy and stenting in symptomatic near-occlusion. http://www.ajnr.org/content/40/7/1207/tab-figures-data
Furthermore, her clinical course suggests high risk of recurrence, although her medical therapy was not previously optimized. Our own data suggests equivalence between endartectomy and stenting in symptomatic near-occlusion. http://www.ajnr.org/content/40/7/1207/tab-figures-data
12/
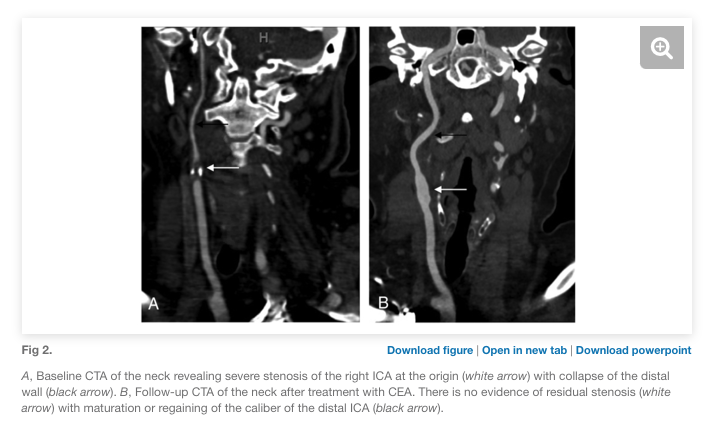
In our series, long-term outcomes showed higher rates of restenosis or asymptomatic interval occlusion than in carotid stenosis without near-occlusion. Still, 79% (stent) and 84% (CEA) had maturation of the revascularized carotid with return of normal vessel caliber.
In our series, long-term outcomes showed higher rates of restenosis or asymptomatic interval occlusion than in carotid stenosis without near-occlusion. Still, 79% (stent) and 84% (CEA) had maturation of the revascularized carotid with return of normal vessel caliber.
Back to our patient: they underwent CEA which was complicated by reflex hypotension. This resolved POD #2 and they were discharged home w/o deficits.
#tweetorial #foamed #neurology #stroke #carotidocclusion #carotidstenosis #endarterectomy #carotidstent #vascularneurology
#tweetorial #foamed #neurology #stroke #carotidocclusion #carotidstenosis #endarterectomy #carotidstent #vascularneurology

 Read on Twitter
Read on Twitter