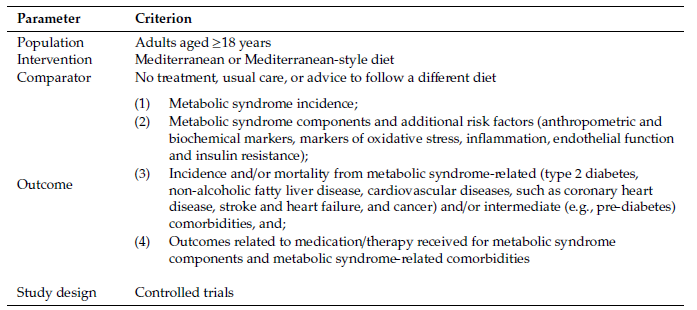
NEW PAPER 
 The Effect of the #Mediterranean #Diet on #Metabolic #Health: A Systematic Review and Meta-Analysis of Controlled Trials in Adults https://www.mdpi.com/2072-6643/12/11/3342 - two months well spent in Boston @harvardmed a year ago with Prof Mantzoros and his team 1/
The Effect of the #Mediterranean #Diet on #Metabolic #Health: A Systematic Review and Meta-Analysis of Controlled Trials in Adults https://www.mdpi.com/2072-6643/12/11/3342 - two months well spent in Boston @harvardmed a year ago with Prof Mantzoros and his team 1/

 The Effect of the #Mediterranean #Diet on #Metabolic #Health: A Systematic Review and Meta-Analysis of Controlled Trials in Adults https://www.mdpi.com/2072-6643/12/11/3342 - two months well spent in Boston @harvardmed a year ago with Prof Mantzoros and his team 1/
The Effect of the #Mediterranean #Diet on #Metabolic #Health: A Systematic Review and Meta-Analysis of Controlled Trials in Adults https://www.mdpi.com/2072-6643/12/11/3342 - two months well spent in Boston @harvardmed a year ago with Prof Mantzoros and his team 1/
What we found 


1. Too limited data to draw conclusions on MetSyn incidence (one study = no risk reduction) - more long-term studies are needed
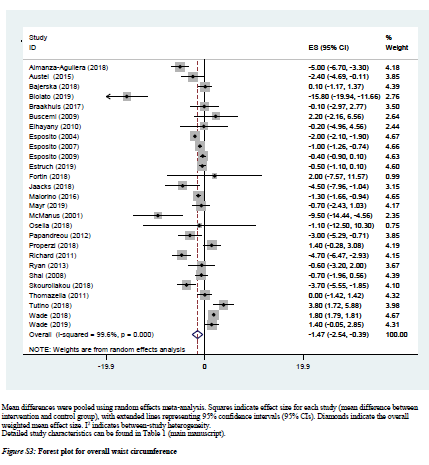
2. Pooled analysis showed that MD had greater beneficial effect on 18 of 28 MetSyn RFs identified (incl all MetSyn components) 3/



1. Too limited data to draw conclusions on MetSyn incidence (one study = no risk reduction) - more long-term studies are needed
2. Pooled analysis showed that MD had greater beneficial effect on 18 of 28 MetSyn RFs identified (incl all MetSyn components) 3/
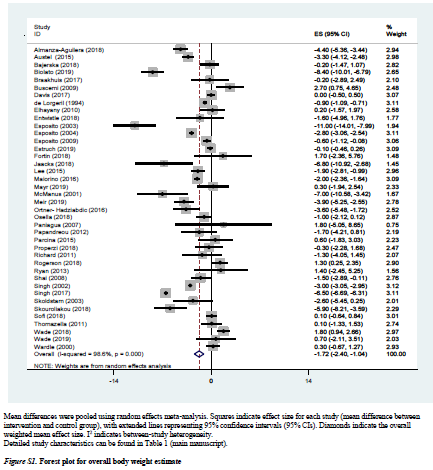
Of note: We confirmed that the MD does not promote increased body weight, in fact the opposite - so #healthcare practitioners should not abstain from promoting the MD to their patients over concerns that it
is ‘fattening' 4/
is ‘fattening' 4/
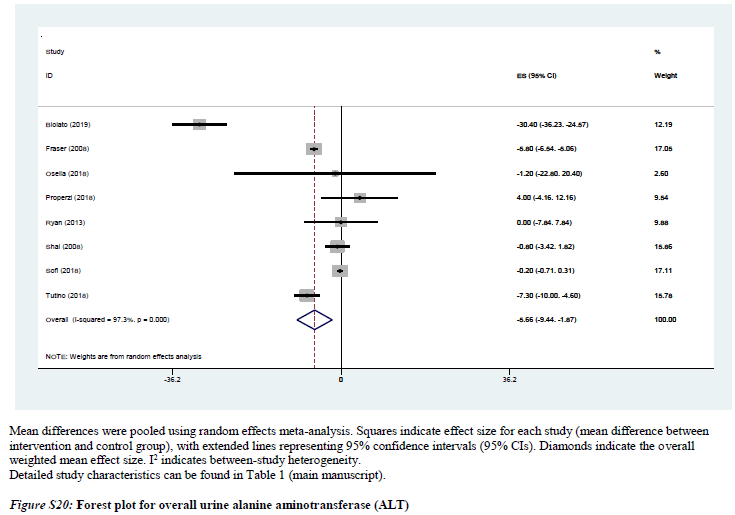
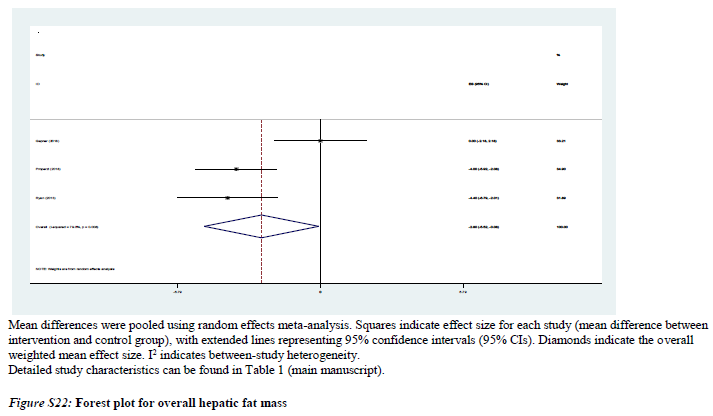
Of note #2: this was the first #metaanalysis to look at #NAFLD outcomes. MD resulted in greater beneficial effects in alanine transaminase concentrations, and hepatic fat mass - we need more studies looking at metabolic outcomes related to NAFLD 5/
Note #3:
Supplementing MD advice with foods from the MD led to beneficial changes in some MetSyn RFs - BUT there was no evidence it leads to greater health benefits beyond those obtained by advice alone = important consideration for MD trial design, esp in non-Med populations 6/
Supplementing MD advice with foods from the MD led to beneficial changes in some MetSyn RFs - BUT there was no evidence it leads to greater health benefits beyond those obtained by advice alone = important consideration for MD trial design, esp in non-Med populations 6/
What we found 

 (cont)
(cont)
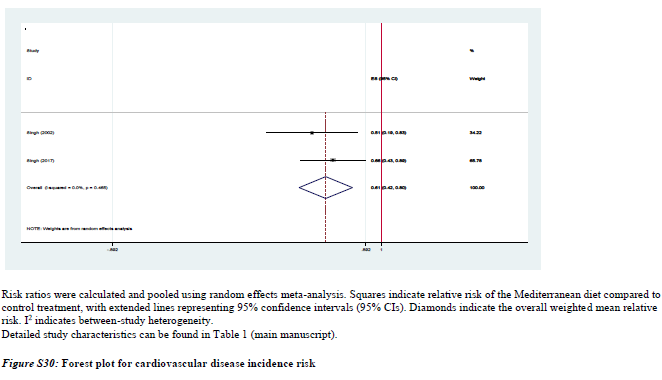
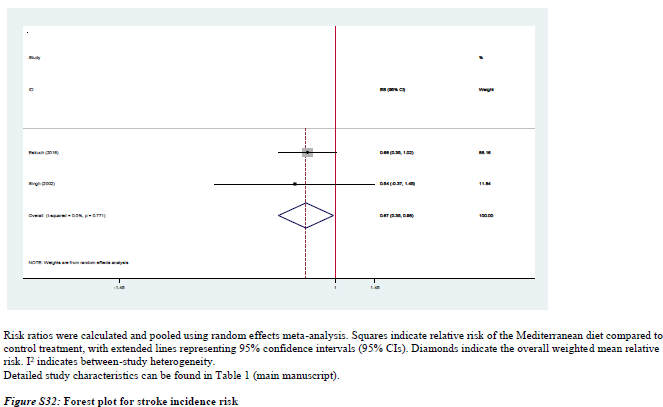
3. The MD resulted in lower risk of CVD and stroke
incidence - no evidence for other hard clinical outcomes but only few such trials available 7/


 (cont)
(cont)3. The MD resulted in lower risk of CVD and stroke
incidence - no evidence for other hard clinical outcomes but only few such trials available 7/
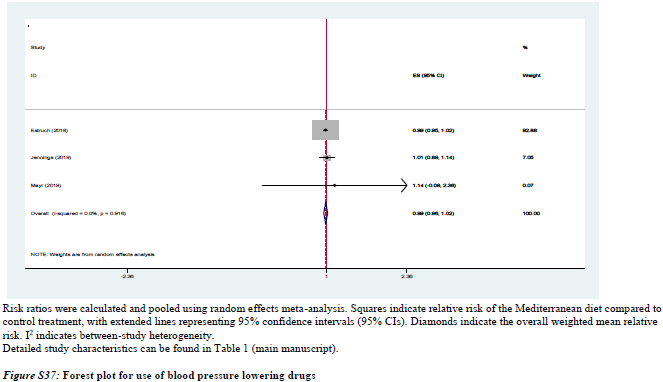
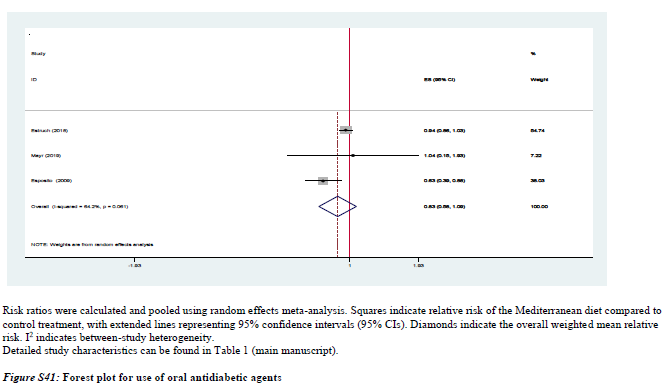
4. Pooled analysis showed no MD effect on the need for pharmacologic treatment for MetSyn or related #comorbidities, eg BP medication or oral anti-diabetic agents. Only one study reported hyperglycaemic drug use as a primary outcome showing a beneficial effect 8/
High heterogeneity in most pooled analyses as expected from complex dietary interventions, so pooled findings should be interpreted with caution; HOWEVER doing the meta-analysis enabled the comparison of findings across studies and the examination of consistency of effects 9/
Most importantly however:
There was a consistent direction of beneficial effect of the MD observed for the vast majority of outcomes examined, so practitioners should not abstain from promoting the #Mediterranean dietary pattern for a wide range of metabolic health benefits 10/
There was a consistent direction of beneficial effect of the MD observed for the vast majority of outcomes examined, so practitioners should not abstain from promoting the #Mediterranean dietary pattern for a wide range of metabolic health benefits 10/
What we need to do to further the field 

1. More long-term #trials with hard clinical + pharmacotherapy outcomes
2. Establish effect of #Mediterranean #diet alone vs. combined with other components, eg energy restriction
3. " Effect of MD alone vs. MD + provision of foods 11/


1. More long-term #trials with hard clinical + pharmacotherapy outcomes
2. Establish effect of #Mediterranean #diet alone vs. combined with other components, eg energy restriction
3. " Effect of MD alone vs. MD + provision of foods 11/
What we need to do to further the field 
 (cont)
(cont)
4. Head-to-head trials examining effect of MD vs. common pharmacologic treatments, e.g. statins or secondary prevention treatments for CVD 12/

 (cont)
(cont)4. Head-to-head trials examining effect of MD vs. common pharmacologic treatments, e.g. statins or secondary prevention treatments for CVD 12/
@LSchwingshackl @JordiSalasSalva @dietamed @HarvardHealth @HNRC_NclUni @BDA_Dietitians @DUK_research @UK_ASO @nutritionorg @dietitiansaus should be of interest - please RT @UoBrisSPS https://www.mdpi.com/2072-6643/12/11/3342 13.

 Read on Twitter
Read on Twitter