Thank you @AndersPerner and co for a nice editorial in @yourICM on the ITACTIC Trial. http://rdcu.be/b9uth
I hope you all won't mind if I give my own view on what ITACTIC means for TEG/ROTEM in trauma.
TL:DR: Use TEG/ROTEM to augment your major haemorrhage protocol. (1/13) https://twitter.com/yourICM/status/1322453119821819904
I hope you all won't mind if I give my own view on what ITACTIC means for TEG/ROTEM in trauma.
TL:DR: Use TEG/ROTEM to augment your major haemorrhage protocol. (1/13) https://twitter.com/yourICM/status/1322453119821819904
I don't think there will ever be another ITACTIC or similar trial. The logistics and complexities were huge. So much like the results of PROPPR, for now we need to take what we can from the ITACTIC results. (2/13)
First, two points of context: A: There were no signals concerning safety. B: The healthcare implications of introducing TEG/ROTEM into trauma are relatively low (A health economics study is in preparation, but this is known). So we can focus on potential clinical benefit: (3/13)
The premise is that treatment of trauma induced coagulopathy (TIC) will improve outcomes. Patients who are not coagulopathic are unlikely to see benefit.
Because we were delivering standard of care TXA/1:1 RBC+FFP, our detected incidence of TIC (by PTr) was 29%. (4/13)
Because we were delivering standard of care TXA/1:1 RBC+FFP, our detected incidence of TIC (by PTr) was 29%. (4/13)
In the coagulopathic subgroup (patients presenting with with PTr>1.2), the observed 28 day mortality was:
Conventional tests (CCT): 55%
TEG/ROTEM (VHA): 41%
For patients who needed a massive transfusion (10+ RBCs), it was:
CCT: 47%
VHA: 38%
Both not significant (5/13)
Conventional tests (CCT): 55%
TEG/ROTEM (VHA): 41%
For patients who needed a massive transfusion (10+ RBCs), it was:
CCT: 47%
VHA: 38%
Both not significant (5/13)
These may be chance findings. The groups aren't stratified. It's impossible to stratify subgroups in this study, etc etc.
BUT what if this difference is real and we were ultimately underpowered because of the lower than expected incidence of TIC? (6/13)
BUT what if this difference is real and we were ultimately underpowered because of the lower than expected incidence of TIC? (6/13)
If the results are real, for patients with TIC, the NNT to save a life would be 7. For patients with massive transfusion, NNT would be 11.
So what do we do?
Ignore this?
Then we get to the surprising outcomes in severe TBI...
(7/13)
So what do we do?
Ignore this?
Then we get to the surprising outcomes in severe TBI...
(7/13)
In the 19% of major haemorrhage patients who also had a severe TBI (AIS Head 4+), 28-day mortality was:
Conventional tests (CCT): 74%
TEG/ROTEM (VHA): 44%
NNT: 3.
Three. For Code Red + Severe TBI. With a baseline mortality of 74%.
This was statistically signficant (8/13)
Conventional tests (CCT): 74%
TEG/ROTEM (VHA): 44%
NNT: 3.
Three. For Code Red + Severe TBI. With a baseline mortality of 74%.
This was statistically signficant (8/13)
For patients with TIC, potentially we could screen for coagulopathy first (?with POC INR) & then decide whether to use TEG/ROTEM or not. Weird but possible.
But you can't screen for TBI. The brain CT is often/usually delayed until after bleeding control. (9/13)
But you can't screen for TBI. The brain CT is often/usually delayed until after bleeding control. (9/13)
And so I think we have to keep working to identify and treat TIC in bleeding trauma patients.
And at the moment I think that's best done by augmenting empiric major haemorrhage protocols with TEG or ROTEM. (10/13)
And at the moment I think that's best done by augmenting empiric major haemorrhage protocols with TEG or ROTEM. (10/13)
There's a lot more to do, examining the ITACTIC data, and with determining the best treatments for TIC.
But my (yes perhaps biased) view is that it's very difficult to say major haemorrhage protocols are best run empirically or augmented with lab tests only. (11/13)
But my (yes perhaps biased) view is that it's very difficult to say major haemorrhage protocols are best run empirically or augmented with lab tests only. (11/13)
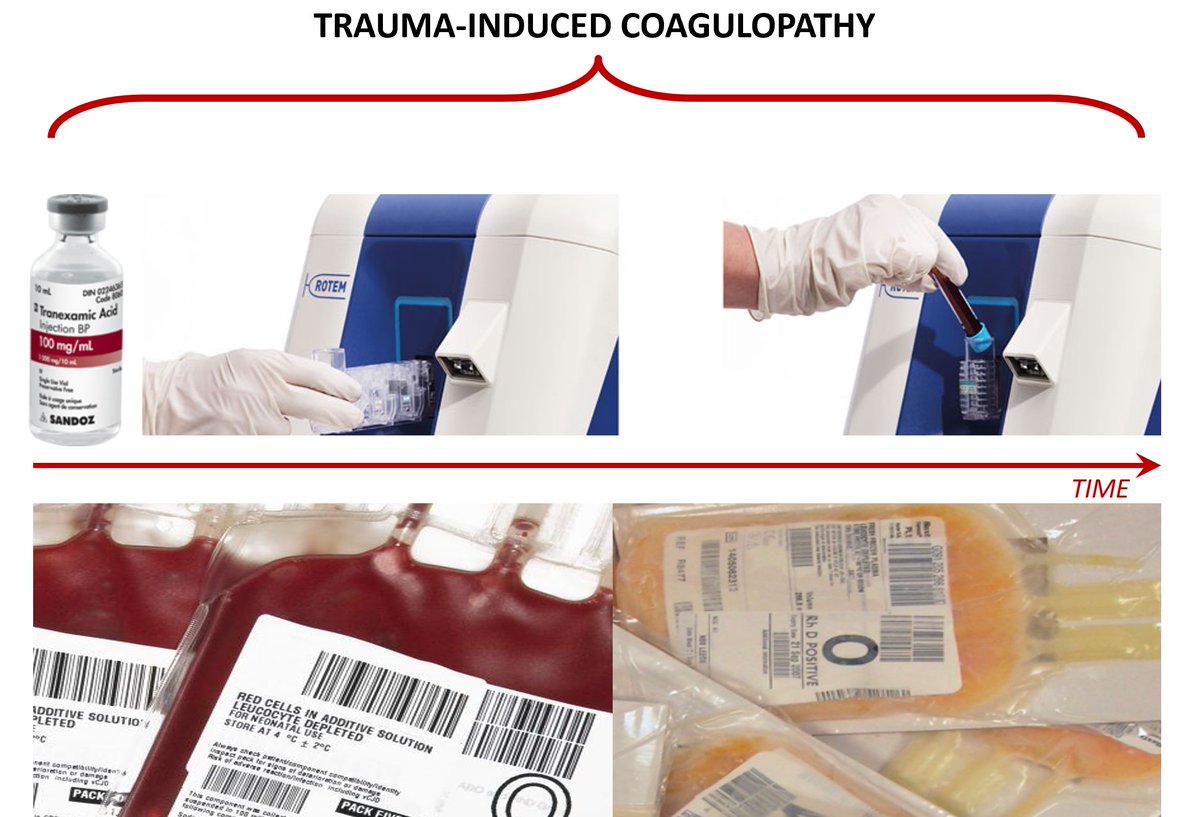
For reference, here's my explainer slide on Trauma Induced Coagulopathy (TIC). Time on the x-axis. TIC =
ATC: Acute Traumatic Coagulopathy
+
Resuscitation induced coagulopathy
+
A late prothrombotic phase in survivors
12/13
ATC: Acute Traumatic Coagulopathy
+
Resuscitation induced coagulopathy
+
A late prothrombotic phase in survivors
12/13
And the ITACTIC concept of hybrid resuscitation:
Give 1:1 RBC+FFP empirically as baseline hroughout to reduce resuscitation coagulopathy
Give TXA and then diagnostic-guided care (CCT or TEG/ROTEM) to identify & treat ATC / developing resuscitation induced coagulopathy. (13/13)
Give 1:1 RBC+FFP empirically as baseline hroughout to reduce resuscitation coagulopathy
Give TXA and then diagnostic-guided care (CCT or TEG/ROTEM) to identify & treat ATC / developing resuscitation induced coagulopathy. (13/13)

 Read on Twitter
Read on Twitter