1/ Thanks - effectively all superspreading events are indoors.
Major risk factors appear to be:
- Poor ventilation, crowding, time, perhaps singing (etc.)
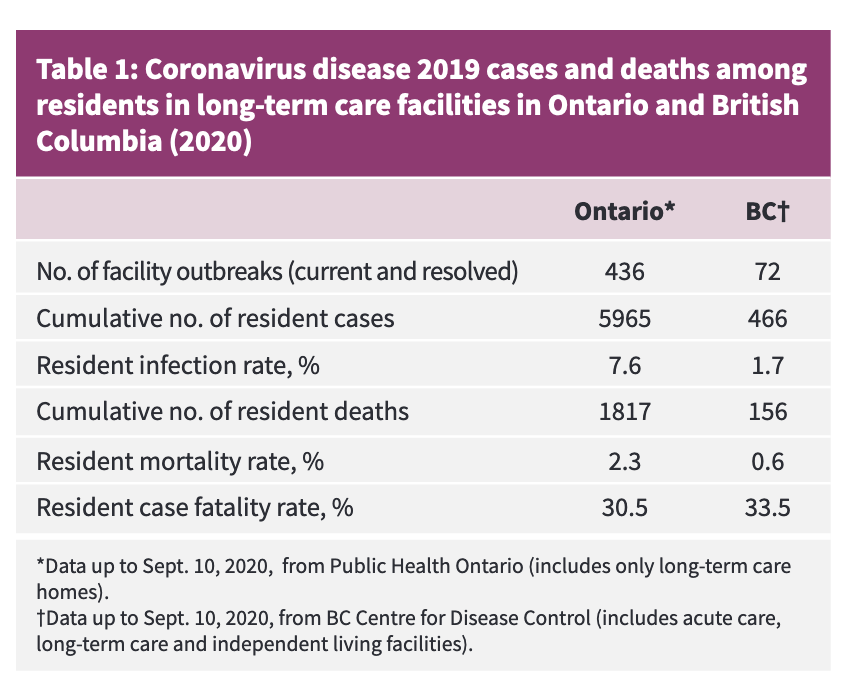
- Vulnerable individuals (hospitals, nursing homes, etc.)
@KoenSwinkels
https://www.stopsuperspread.com/p/infographic.html https://twitter.com/Maxwellll12/status/1319484859274776578
Major risk factors appear to be:
- Poor ventilation, crowding, time, perhaps singing (etc.)
- Vulnerable individuals (hospitals, nursing homes, etc.)
@KoenSwinkels
https://www.stopsuperspread.com/p/infographic.html https://twitter.com/Maxwellll12/status/1319484859274776578
2/ My view is that #covid19 policy should encourage people to be outdoors as much as possible.
Less: policing of outdoor behaviour, non-specific contact tracing
More: preventing clusters in hospitals & nursing homes, ventilation upgrades, contact tracing focused on clusters
Less: policing of outdoor behaviour, non-specific contact tracing
More: preventing clusters in hospitals & nursing homes, ventilation upgrades, contact tracing focused on clusters
3/ Focusing on preventing clusters can be more successful than many people think
e.g., different nursing home policies in two different provinces in Canada led to stark differences in outcomes with many deaths prevented
Probably also true for hospitals
https://www.cmaj.ca/content/cmaj/early/2020/09/29/cmaj.201860.full.pdf
e.g., different nursing home policies in two different provinces in Canada led to stark differences in outcomes with many deaths prevented
Probably also true for hospitals
https://www.cmaj.ca/content/cmaj/early/2020/09/29/cmaj.201860.full.pdf
4/ There has also been interesting differences in tracing policies in places like Japan - which focused more on identifying clusters / superspreading events
These were lessons from SARS as well as tuberculosis https://asiatimes.com/2020/06/japans-contact-tracing-method-is-old-but-gold/
These were lessons from SARS as well as tuberculosis https://asiatimes.com/2020/06/japans-contact-tracing-method-is-old-but-gold/
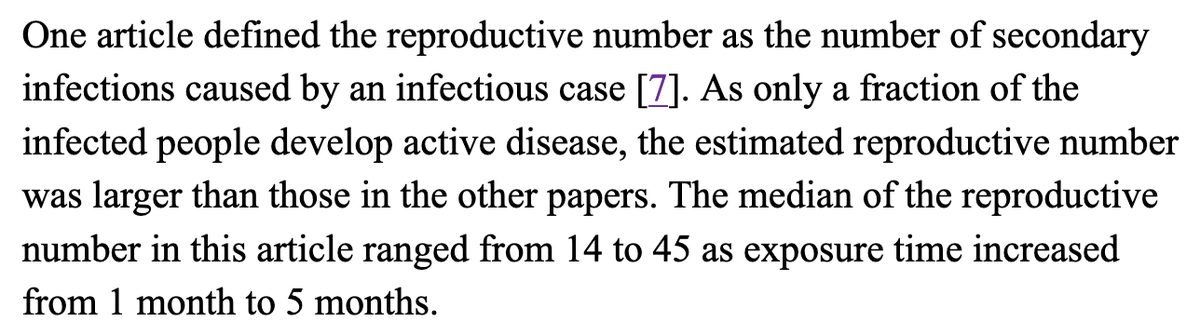
5/ @JoshOsowicki put me on to this great study of tuberculosis (TB) transmission
The R for active TB cases leading to latent TB was estimated to be 14-45 (huge!)
https://asiatimes.com/2020/06/japans-contact-tracing-method-is-old-but-gold/
The R for active TB cases leading to latent TB was estimated to be 14-45 (huge!)
https://asiatimes.com/2020/06/japans-contact-tracing-method-is-old-but-gold/
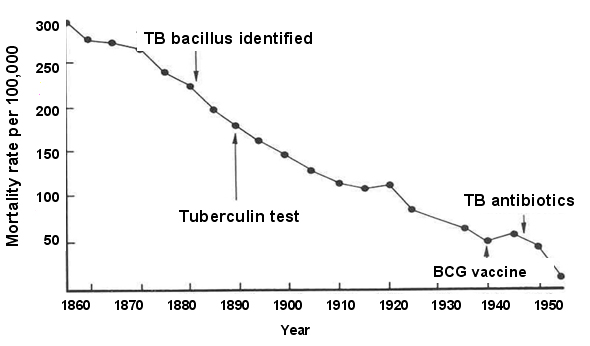
6/ Public health learned lessons about TB >100 years ago
Addressing social factors like overcrowding, poor ventilation, poverty made a big difference (perhaps more than treatment or a vaccine -see below)
We probably need more of this old school public health approach right now
Addressing social factors like overcrowding, poor ventilation, poverty made a big difference (perhaps more than treatment or a vaccine -see below)
We probably need more of this old school public health approach right now
7/ There is sometimes too much focus on individual 'superspreaders', when we should focus instead on context (factors that promote super-spreading events)
If a superspreader lives in a forest, do they infect anyone?
cc'ing @prof_goldberg
If a superspreader lives in a forest, do they infect anyone?
cc'ing @prof_goldberg

 Read on Twitter
Read on Twitter