When #COVID19 plowed through NYC like a tidal wave, the chances of survival heavily depended on the hospital you were treated in. In hard hit outer borough/public hospitals, the mortality rate was 3x higher than Manhattan private hospitals. A thread: https://www.nytimes.com/2020/07/01/nyregion/Coronavirus-hospitals.html
2/ Hospitals in Queens, Brooklyn, the Bronx, and Upper Manhattan quickly became overwhelmed given that they serve lower income patients at higher risk of getting infected with #COVID19. A single nurse may have been responsible for 15-20 patients, when 3-6 is the norm
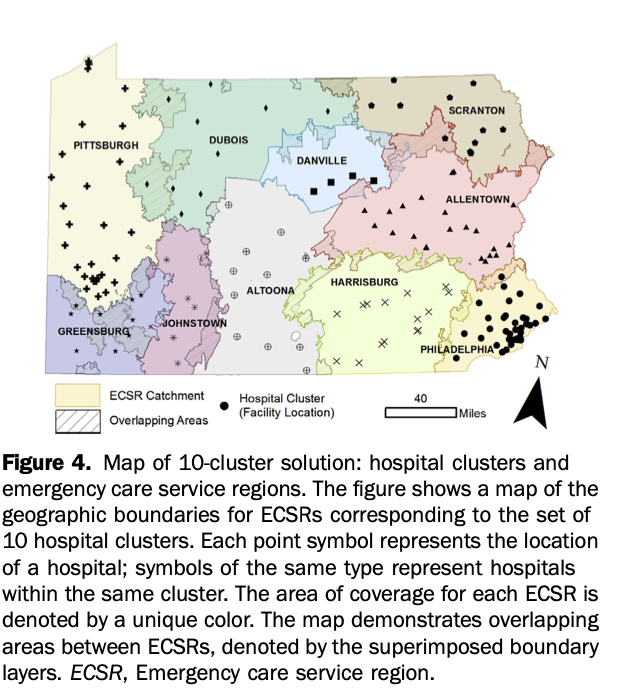
3/ While these hospitals were strained beyond capacity, others a few miles away were less strained. This begs the question, why weren't patients sent by ambulance to less strained hospitals and why weren't they transferred there if they landed at an overwhelmed hospital?
4/ Despite mortality rates 3x higher and being strained beyond capacity contributing to the total of 17,500 deaths in NYC, less than *50* patients were transferred out of public hospitals to private hospitals https://www.nytimes.com/2020/07/27/podcasts/the-daily/new-york-hospitals-covid.html?showTranscript=1
5/ The underlying reasons are longstanding and need to be addressed:
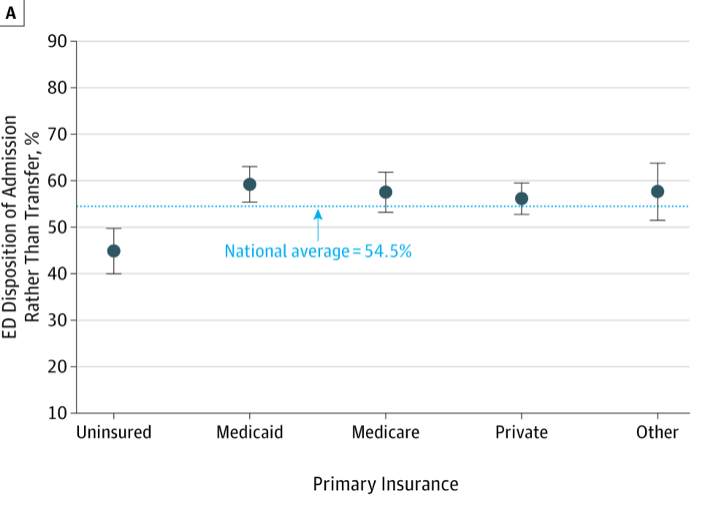
1) How acute care is financed and the incentives it creates based on the ownership/affiliation of the hospital and the insurance status of the patient
2) (Lack of) coordination of ambulances/transfers
1) How acute care is financed and the incentives it creates based on the ownership/affiliation of the hospital and the insurance status of the patient
2) (Lack of) coordination of ambulances/transfers
6/ Basically, public hospitals have an incentive not to transfer out patients with insurance and private hospitals have a disincentive to not accept transfers of patients without insurance. Therefore, there is no pre-existing infrastructure to coordinate these transfers
7/ This is a national problem. In my prior work, I showed that U.S. patients with severe injuries that landed at community hospital were significantly less likely to be transferred out to a trauma center if they had insurance
https://www.npr.org/sections/health-shots/2014/02/19/279709454/insurance-not-injuries-may-determine-who-goes-to-trauma-centers
https://www.npr.org/sections/health-shots/2014/02/19/279709454/insurance-not-injuries-may-determine-who-goes-to-trauma-centers
8/ Real-time dashboards can show hospital capacity strain and ability to receive new patients and guide ambulances to less strained hospitals. The tech is old and it works as shown in this 2010 Canadian study. However, few U.S. regions use these systems https://pubmed.ncbi.nlm.nih.gov/21122023/
9/ It's inevitable that we will be faced with another disaster and our high risk regions are the ones where ERs and hospitals are already stretched to capacity on a daily basis. See prior thread: https://twitter.com/kit_delgadoMD/status/1236388778811576324?s=20
10/ So being ready for the next surge starts now. As @Dr_BrendanCarr has said for a while, "form follows finance" when creating regional health systems that are prepared to surge to meet demand: https://www.modernhealthcare.com/opinion-editorial/creating-culture-readiness-within-healthcare-system
11/ Models exist for getting private-public entities to rapidly pull together to address disasters. Think utility companies surging to storm hit areas https://twitter.com/kit_delgadoMD/status/1283763848697315330?s=20
12/ Getting @CMSGov to incentivize hospitals in regions to coordinate transfers/care to achieve the best possible outcomes for patients with emergency conditions is one way to get closer to a more functional emergency care system.
https://www.jefferson.edu/content/dam/university/research/lab-assets/Carr/QualityThroughCoopetition.pdf
https://www.jefferson.edu/content/dam/university/research/lab-assets/Carr/QualityThroughCoopetition.pdf
13/ And finally, given that overwhelmed hospitals disproportionally serve lower income, Black and Latino patients, coordinating regional readiness, emergency response, and transfers to distribute the surge is key for reducing racial disparities in care and outcomes
end/
end/
Tagging colleagues that have been thinking about hospital readiness, financing, surge, and racial disparities
@oziadias @UREssien @terwiesch @kevin_volpp @Eugenia_South @UtshaKhatriMD @AriBFriedman @bernardchangMD @Craig_A_Spencer @DrMichelleLin @LauraBurke20 @AmolNavathe
@oziadias @UREssien @terwiesch @kevin_volpp @Eugenia_South @UtshaKhatriMD @AriBFriedman @bernardchangMD @Craig_A_Spencer @DrMichelleLin @LauraBurke20 @AmolNavathe

 Read on Twitter
Read on Twitter