Last Sunday,I presented a bacterial meningitis due to S.suis to amazing teachers and friends in the VMR students of the CPsolvers @CPSolvers.
#MedTwitter #MedStudentTwitter
#MedTwitter #MedStudentTwitter
Thank you Dr. Anand @Anand_88_Patel, Dr. Daniel @dminter89, Kiara @kiaracamacho96, Dhruv @TheRealDSrini, Andrea @AndreaAnampaGand, Sukriti @sukritibanthiya and friends in the chat box for amazing discussion.
Today, I create some tweetorials that talk about a little bit of bacterial meningitis and S.suis.
I hope Rumi will enjoy it, Dr. Rabih @rabihmgeha.
I hope Rumi will enjoy it, Dr. Rabih @rabihmgeha.
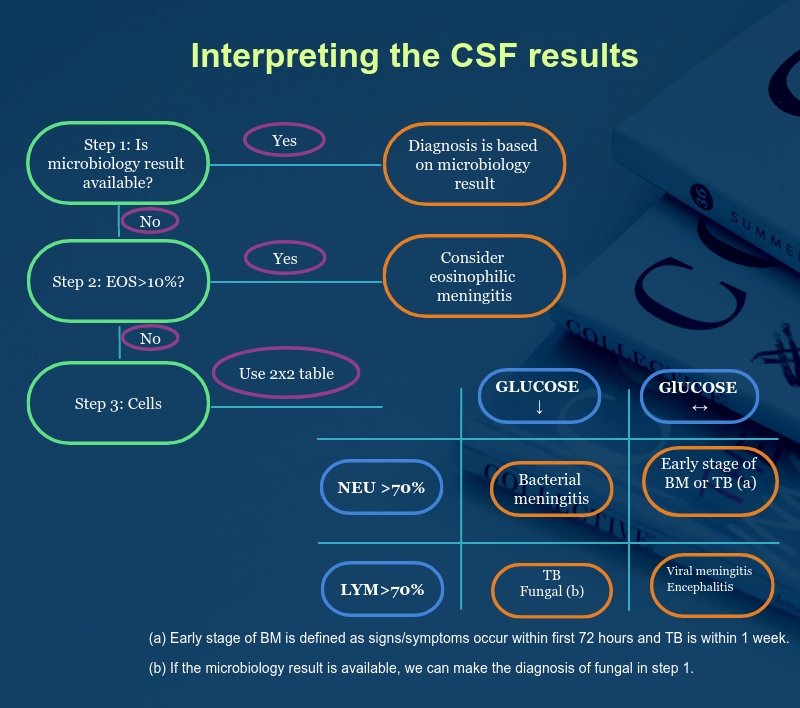
Secondly, here are some information about bacterial meningitis (BM).
BM is a neurologic emergency which require rapid diagnosis and treatment.
Source: Mandell Douglas and Bennett's Principles and Practice of Infectious Diseases, chapter 89-Acute Bacterial Meningitis, page 1097
BM is a neurologic emergency which require rapid diagnosis and treatment.
Source: Mandell Douglas and Bennett's Principles and Practice of Infectious Diseases, chapter 89-Acute Bacterial Meningitis, page 1097
Now I will talk about Streptococcus Suis (S.suis) which is the most common agent that causes BM in Vietnam. Besides, I will put the patient's case to compare between the literature and clinical practice.
S.suis is gram- positive facultatively anaerobic.
There are 33- 35 serotypes of S.suis were detectable,
serotype 2 was the most common agents.
Pigs are considered as natural reservoir of S.suis and the main source of human infection.
are considered as natural reservoir of S.suis and the main source of human infection.
There are 33- 35 serotypes of S.suis were detectable,
serotype 2 was the most common agents.
Pigs
 are considered as natural reservoir of S.suis and the main source of human infection.
are considered as natural reservoir of S.suis and the main source of human infection.
 Epidemology
EpidemologyLocation: Worldwide, emerging bacterial pathogen in Asia
Sex: male (82%)
Mean age: 49
In adults
Overall, S. suis serotype 2 is the most common agent that causes BM in the adult group of Southern Vietnam: 49%
<30 years old: S. suis causes <9% of BM cases
>30 years old: S.suis causes 61% of BM cases
In children: S.suis was not isolated from pediatric patients.
Overall, S. suis serotype 2 is the most common agent that causes BM in the adult group of Southern Vietnam: 49%
<30 years old: S. suis causes <9% of BM cases
>30 years old: S.suis causes 61% of BM cases
In children: S.suis was not isolated from pediatric patients.
 Risk factor
Risk factorOccupational exposures (<50% cases in Asia): slaughter house workers, butchers, pig breeders, meat processing, and pig transport.
Behaviour related risk factor: ingestion of high risk contaminated pig food: fresh or undercooked blood, tonsils, tongue, stomach, intestines and uterus.
Host: minor cuts or abrasions on their skin: 33%
Bones of pig are very sharp, so sometimes it may cause tiny injuries in hands of patients that physicians can not see clearly. Therefore, examination especially in hands is very important.
Bones of pig are very sharp, so sometimes it may cause tiny injuries in hands of patients that physicians can not see clearly. Therefore, examination especially in hands is very important.

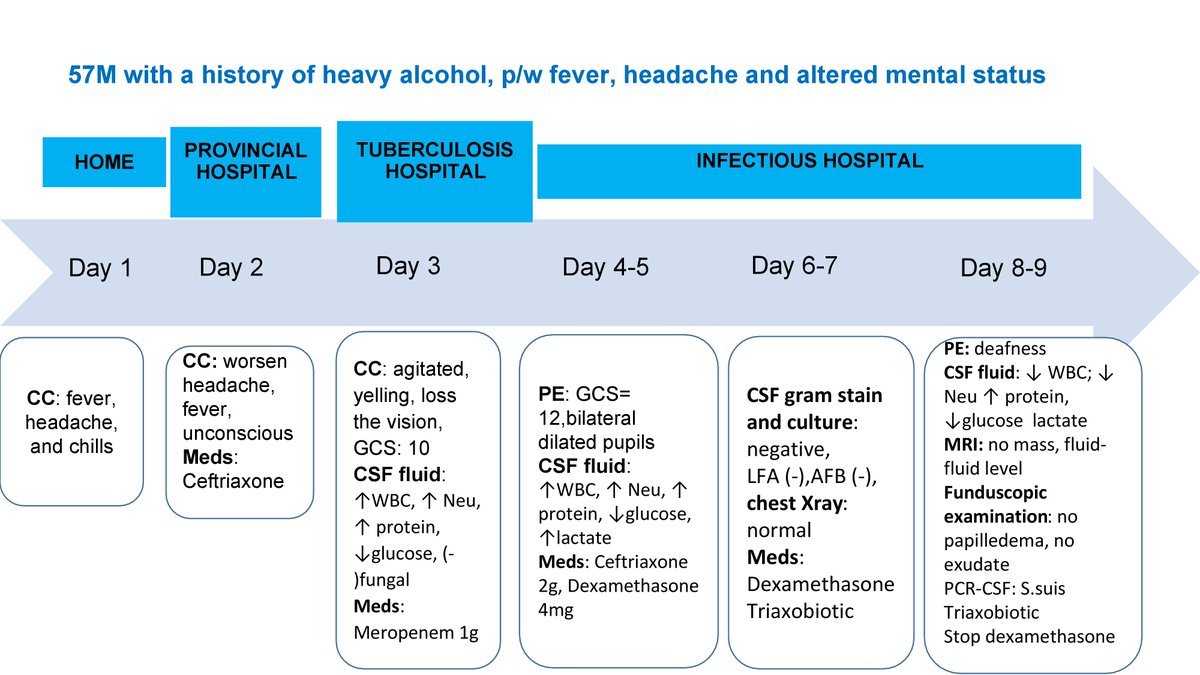
Patient's case
He lived in South Vietnam and his age was 57.
He was a rice farmer, and he didn’t do any jobs related to pigs. However, there is one more way for S.suis to transmit is the GI tract. We didn’t know whether he had eaten fresh blood or the intestines of the pigs.
He lived in South Vietnam and his age was 57.
He was a rice farmer, and he didn’t do any jobs related to pigs. However, there is one more way for S.suis to transmit is the GI tract. We didn’t know whether he had eaten fresh blood or the intestines of the pigs.
In Vietnam, fresh pig blood or chicken blood was quiet popular for previous decades. Nowadays, there is a reduction in the number of people living in urban areas who eat fresh blood, but there may still be a popular dishes in people who live in rural areas.
Clinical manifestation
Incubation period: median 2.2 days (Sichuan, China)
 Neurology: meningitis, epidural abscess, spondylodiscitis
Neurology: meningitis, epidural abscess, spondylodiscitis
 Ears: Hearing loss is striking signs of S.suis
Ears: Hearing loss is striking signs of S.suis
 Eyes: endophthalmitis, uveitis ophthalmoplegia
Eyes: endophthalmitis, uveitis ophthalmoplegia
 Cardiovascular: endocarditis
Cardiovascular: endocarditis
Incubation period: median 2.2 days (Sichuan, China)
 Neurology: meningitis, epidural abscess, spondylodiscitis
Neurology: meningitis, epidural abscess, spondylodiscitis  Ears: Hearing loss is striking signs of S.suis
Ears: Hearing loss is striking signs of S.suis  Eyes: endophthalmitis, uveitis ophthalmoplegia
Eyes: endophthalmitis, uveitis ophthalmoplegia Cardiovascular: endocarditis
Cardiovascular: endocarditis
Skin: very important. There are 2 things to do:
 Examine for injuries, take physical examination carefully in hands and feet. Sometimes, we don't see the injuries b/c it is too small.
Examine for injuries, take physical examination carefully in hands and feet. Sometimes, we don't see the injuries b/c it is too small.
 Examine rash: petechiae, purpura, and ecchymoses, ganerage in the finger and toes (rare)
Examine rash: petechiae, purpura, and ecchymoses, ganerage in the finger and toes (rare)
 Examine for injuries, take physical examination carefully in hands and feet. Sometimes, we don't see the injuries b/c it is too small.
Examine for injuries, take physical examination carefully in hands and feet. Sometimes, we don't see the injuries b/c it is too small. Examine rash: petechiae, purpura, and ecchymoses, ganerage in the finger and toes (rare)
Examine rash: petechiae, purpura, and ecchymoses, ganerage in the finger and toes (rare)
 Musculoskeletal: acute pyogenic arthritis
Musculoskeletal: acute pyogenic arthritis  Serve disease: toxic shock syndrome
Serve disease: toxic shock syndromeAcute renal failure, acute respiratory distress, consumptive coagulopathy
Patient's case
He had fever, headache, and AMS but the nuchal rigidity is not clear. No signs of toxic shock syndrome as well.
We didn’t find skin injuries in his hands and his feet. Furthermore, there was not any rash in his extremities.
He had fever, headache, and AMS but the nuchal rigidity is not clear. No signs of toxic shock syndrome as well.
We didn’t find skin injuries in his hands and his feet. Furthermore, there was not any rash in his extremities.
There is no clear that he had cranial nerve palsies (III, IV, VI and VII). On the day number 9, physical examination revealed his deafness.
 Microbiology disagnosis
Microbiology disagnosisCSF or blood culture: often misidentified or negative as a result of prior antibiotics.
Serotype 2- specific PCR CSF (gen targeted: cps2J) will improve the diagnosis.
In a case series which are conducted in Ho Chi Minh city, Vietnam, there are 117/151 patient were detected to have positive CSF culture and 149/151 patients were detected to have positive real- time PCR.
His first and second CSF results were consistent with bacterial meningitis. However, the CSF and blood culture (on the day number 6) was negative. And PCR CSF result identified S.suis on the day number 9.
 Treatment
TreatmentAntibiotics: Ceftriaxone
Adjunctive therapy: Dexamethason, controversial, just give when TB is excluded.
More sources:
https://www.nejm.org/doi/10.1056/NEJMoa070852
https://www.nejm.org/doi/full/10.1056/nejmoa021334
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4624688/
https://academic.oup.com/cid/article/48/5/617/388486
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3050921/https://pubmed.ncbi.nlm.nih.gov/19413493/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4624688/
https://academic.oup.com/cid/article/48/5/617/388486
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3050921/https://pubmed.ncbi.nlm.nih.gov/19413493/
If it is inconvenience for you to read tweetorial, I put them together in this drive link:
https://drive.google.com/drive/folders/1SEHiEvWZFgVG8LI1mIF80_rYVgbmk3tw?usp=sharing
https://drive.google.com/drive/folders/1SEHiEvWZFgVG8LI1mIF80_rYVgbmk3tw?usp=sharing

 Read on Twitter
Read on Twitter