1/ TIL about acquired hemophilia A (AH), a condition in which an auto-antibody of factor VIII is formed resulting in profound risk of bleeding. Early suspicion and treatment are critical to avoid procedures and to eradicate this inhibitor.
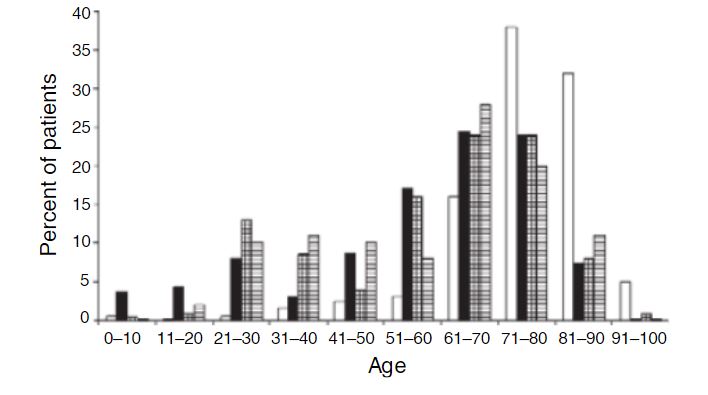
2/ Mortality is high in AH, in part due to the difficulty of diagnosis. AH most commonly presents in individuals >60yo or in young mothers in the postpartum period. The clinical presentation isn’t the same as hemophilia A, either.
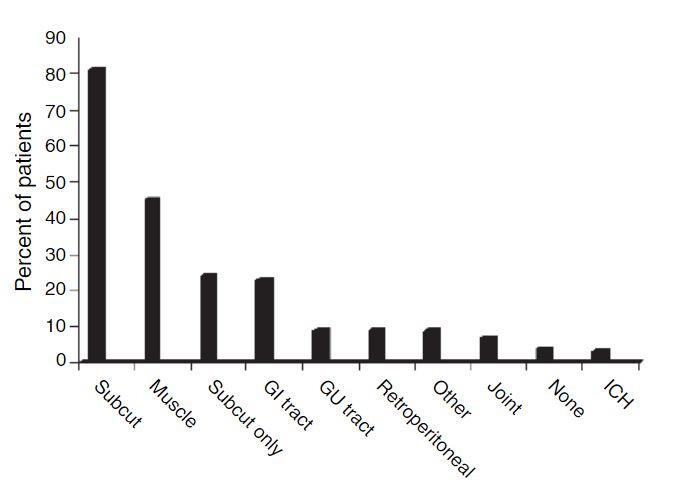
3/ Patients commonly present with hemorrhages into the skin, soft tissues, or mucus membranes rather than joints like Hemophilia A/B. In mothers, prolong postpartum bleeding can be the primary presentation.
4/ An isolated PTT is seen which doesn’t correct with a mixing study like a deficiency would. Lupus anticoagulant and heparin use must be excluded. A lack of a family history can often lead to complex testing.
5/ Treatment of the inhibitor depends on the titer, such that lower titer inhibitors can be “overcome” with sufficient dosing of Factor VIII. Strong inhibitors need to be bypassed with recombinant factors such as FEIBA or recombinant factor VIIa.
6/ Apheresis or immunoadsorption procedures for coagulation inhibitors are an ASFA category III indication. The mainstay of chronic therapy is immunosuppression to “tamp down” the responsible autoimmune response.
7/ While somewhat out of my wheelhouse, I would welcome a discussion on tolerance induction for these inhibitors from those with a better understanding of its practice and efficacy!

 Read on Twitter
Read on Twitter