1/
72F with CML had persistent fever ~102F, cough. CT chest with focal consolidation in LLL. Sputum cx: Klebsiella pneumoniae. Serum BDG, GM negative.
Was on Vanc/Cefepime/LAmB, now narrowed to Cefepime + afebrile 24h
Duration of Cefepime?
#IDTwitter #IDMedEd #IDFellows
72F with CML had persistent fever ~102F, cough. CT chest with focal consolidation in LLL. Sputum cx: Klebsiella pneumoniae. Serum BDG, GM negative.
Was on Vanc/Cefepime/LAmB, now narrowed to Cefepime + afebrile 24h
Duration of Cefepime?
#IDTwitter #IDMedEd #IDFellows
Today’s #tweetorial is on fever + neutropenia!
Background:
Up to 50% pts with solid tumors & >80% pts with hem malignancy will develop fever during chemo cycle assoc’d with neutropenia
Only 20-30% of these identify clinical infection
Only 10-25% bacteremia
Background:
Up to 50% pts with solid tumors & >80% pts with hem malignancy will develop fever during chemo cycle assoc’d with neutropenia
Only 20-30% of these identify clinical infection
Only 10-25% bacteremia
3/
The very basics:
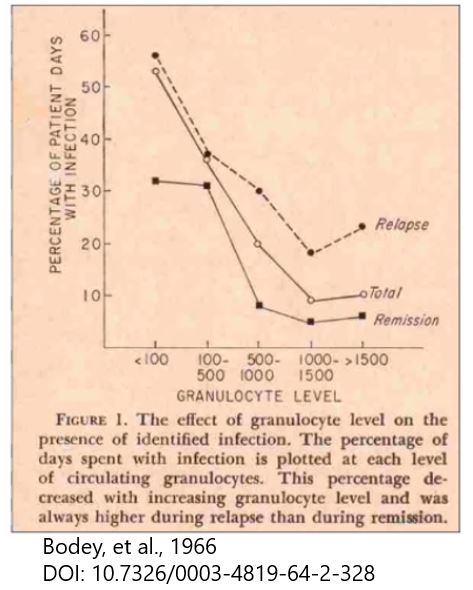
 Here is the classic article from 1966 that demonstrated
Here is the classic article from 1966 that demonstrated  susc to infection as neutrophils<500
susc to infection as neutrophils<500
 Freq and severity of infection inversely proportional to neutrophil count
Freq and severity of infection inversely proportional to neutrophil count
 Risk of severe infection and BSI greatest at ANC <100
Risk of severe infection and BSI greatest at ANC <100
https://pubmed.ncbi.nlm.nih.gov/5216294/
The very basics:
 Here is the classic article from 1966 that demonstrated
Here is the classic article from 1966 that demonstrated  susc to infection as neutrophils<500
susc to infection as neutrophils<500 Freq and severity of infection inversely proportional to neutrophil count
Freq and severity of infection inversely proportional to neutrophil count Risk of severe infection and BSI greatest at ANC <100
Risk of severe infection and BSI greatest at ANC <100https://pubmed.ncbi.nlm.nih.gov/5216294/
4/
Now setting the definitions straight:
 Fever = Single temp >=38.3C or >=38 sustained over 1 hr period
Fever = Single temp >=38.3C or >=38 sustained over 1 hr period
 Neutropenia = <500 neutrophils/microL or <1000 with predicted decline to <500 over next 48 hrs
Neutropenia = <500 neutrophils/microL or <1000 with predicted decline to <500 over next 48 hrs
First Q: Can pts ever be treated outpatient with PO abxs for F&N?
Now setting the definitions straight:
 Fever = Single temp >=38.3C or >=38 sustained over 1 hr period
Fever = Single temp >=38.3C or >=38 sustained over 1 hr period Neutropenia = <500 neutrophils/microL or <1000 with predicted decline to <500 over next 48 hrs
Neutropenia = <500 neutrophils/microL or <1000 with predicted decline to <500 over next 48 hrsFirst Q: Can pts ever be treated outpatient with PO abxs for F&N?
5/
 Possibly, if anticipate brief neutropenia + no/few co-morbidities
Possibly, if anticipate brief neutropenia + no/few co-morbidities
 High vs low risk according to NCCN + IDSA guidelines are below (notice a lot of overlap)
High vs low risk according to NCCN + IDSA guidelines are below (notice a lot of overlap)
 In addition, there is a formal risk classification = MASCC score (
In addition, there is a formal risk classification = MASCC score ( for details)
for details)
 Low risk >=21
Low risk >=21
 High risk <21
High risk <21
 Possibly, if anticipate brief neutropenia + no/few co-morbidities
Possibly, if anticipate brief neutropenia + no/few co-morbidities High vs low risk according to NCCN + IDSA guidelines are below (notice a lot of overlap)
High vs low risk according to NCCN + IDSA guidelines are below (notice a lot of overlap) In addition, there is a formal risk classification = MASCC score (
In addition, there is a formal risk classification = MASCC score ( for details)
for details) Low risk >=21
Low risk >=21 High risk <21
High risk <21
6/
Initial empiric F&N tx (NCCN/IDSA) = monotherapy w/ anti-pseudomonal beta-lactam:
 Cefepime, Imi/Cilast, Mero, Pip-Tazo
Cefepime, Imi/Cilast, Mero, Pip-Tazo
 Ceftaz (but NCCN category 2B,
Ceftaz (but NCCN category 2B,  GPC activity,
GPC activity,  breakthrough inf)
breakthrough inf)
Oral abxs if low-risk: Cipro+Amox/Clav, Moxiflox, Levoflox
But also think about
Initial empiric F&N tx (NCCN/IDSA) = monotherapy w/ anti-pseudomonal beta-lactam:
 Cefepime, Imi/Cilast, Mero, Pip-Tazo
Cefepime, Imi/Cilast, Mero, Pip-Tazo Ceftaz (but NCCN category 2B,
Ceftaz (but NCCN category 2B,  GPC activity,
GPC activity,  breakthrough inf)
breakthrough inf)Oral abxs if low-risk: Cipro+Amox/Clav, Moxiflox, Levoflox
But also think about

7/
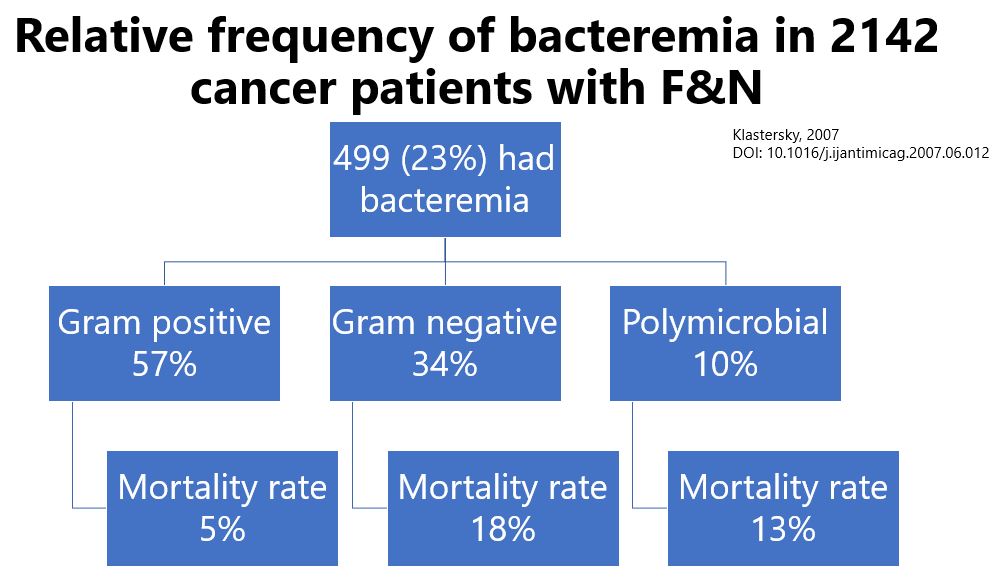
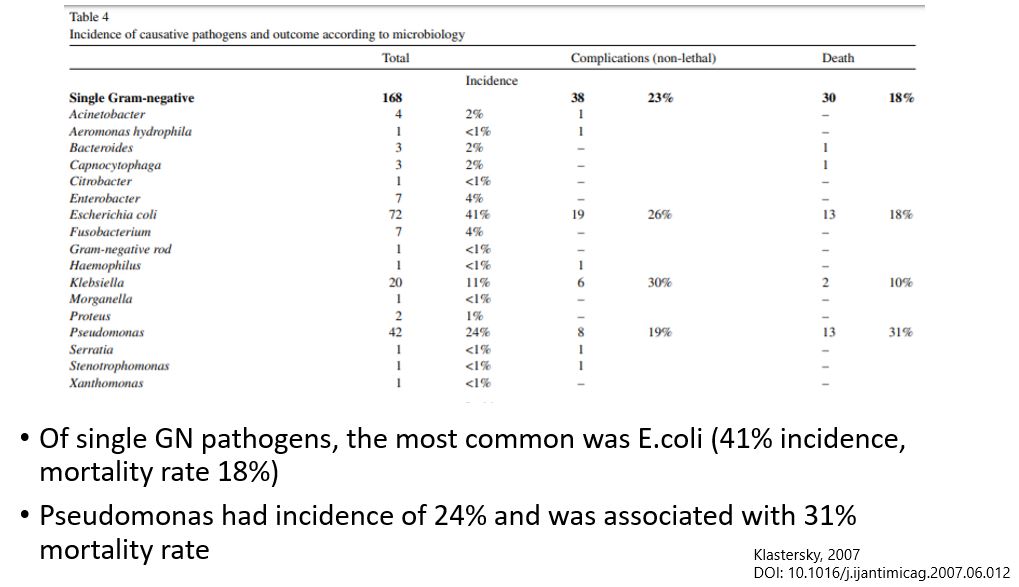
Why target with anti-pseudomonal therapy?
 Goal of initial empiric therapy = prevent serious M&M fr bact until further cx data available
Goal of initial empiric therapy = prevent serious M&M fr bact until further cx data available
 GN organisms, esp Pseudomonas, associated with high complication and mortality rate
GN organisms, esp Pseudomonas, associated with high complication and mortality rate
 Highlighted below:
Highlighted below:
https://pubmed.ncbi.nlm.nih.gov/17689933/
Why target with anti-pseudomonal therapy?
 Goal of initial empiric therapy = prevent serious M&M fr bact until further cx data available
Goal of initial empiric therapy = prevent serious M&M fr bact until further cx data available GN organisms, esp Pseudomonas, associated with high complication and mortality rate
GN organisms, esp Pseudomonas, associated with high complication and mortality rate Highlighted below:
Highlighted below:https://pubmed.ncbi.nlm.nih.gov/17689933/
8/
When to consider additional GP coverage (see image below)
Now, when to consider stopping this GP tx?
Should discontinue 2-3d later if no GP organism is identified! Study about this in next tweet
When to consider additional GP coverage (see image below)
Now, when to consider stopping this GP tx?
Should discontinue 2-3d later if no GP organism is identified! Study about this in next tweet
9/
https://pubmed.ncbi.nlm.nih.gov/2019772/
747 F&N pts randomized to ceftaz+amikacin +/- vanc as initial therapy
 No diff by tx regimen in proportion of febrile pts on each day or in fever duration
No diff by tx regimen in proportion of febrile pts on each day or in fever duration
 No pt with GP BSI died during 1st 3d
No pt with GP BSI died during 1st 3d

 nephrotox if tx'd with vanc (6% vs 2%)
nephrotox if tx'd with vanc (6% vs 2%)
https://pubmed.ncbi.nlm.nih.gov/2019772/
747 F&N pts randomized to ceftaz+amikacin +/- vanc as initial therapy
 No diff by tx regimen in proportion of febrile pts on each day or in fever duration
No diff by tx regimen in proportion of febrile pts on each day or in fever duration No pt with GP BSI died during 1st 3d
No pt with GP BSI died during 1st 3d
 nephrotox if tx'd with vanc (6% vs 2%)
nephrotox if tx'd with vanc (6% vs 2%)
10/
Duration of abxs are dictated by the organism and site of infection.
Recommendations on when to de-escalate in those with w/o source varies slightly by organization
So, what is safety of early d/c of abxs in these pts vs continuing until resolution of neutropenia??
Duration of abxs are dictated by the organism and site of infection.
Recommendations on when to de-escalate in those with w/o source varies slightly by organization

So, what is safety of early d/c of abxs in these pts vs continuing until resolution of neutropenia??
11/
There is a Cochrane review of this that examined 8 RCTs. Between short vs long abxs arms, no difference in all-cause mortality, rates of clinical failure, incidence of BSI - but made no strong conclusions as evidence is limited by imprecision, selection bias, variable defns
There is a Cochrane review of this that examined 8 RCTs. Between short vs long abxs arms, no difference in all-cause mortality, rates of clinical failure, incidence of BSI - but made no strong conclusions as evidence is limited by imprecision, selection bias, variable defns
12/
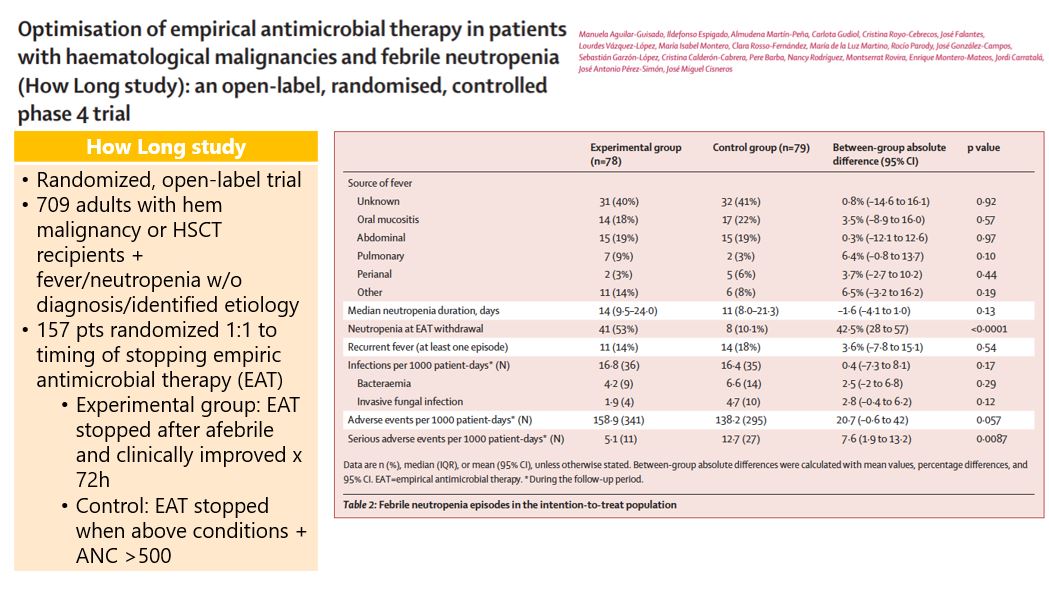
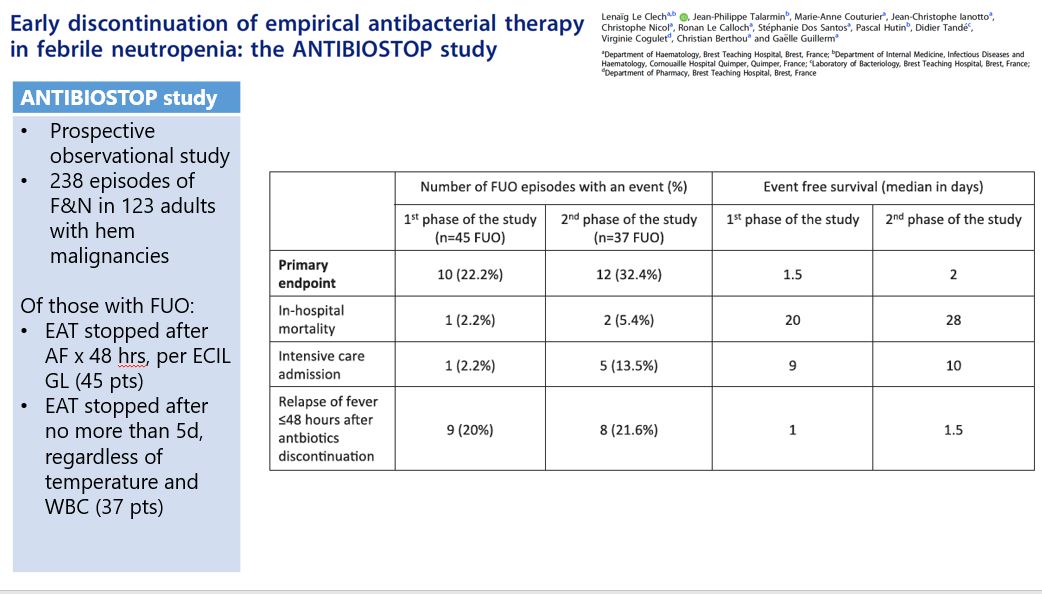
2 papers you can look at when thinking about feasibility and safety of short term abx treatment:
How Long study (was included in Cochrane review)
https://pubmed.ncbi.nlm.nih.gov/29153975/
ANTIBIOSTOP study …https://pubmed-ncbi-nlm-nih-gov.ezp-prod1.hul.harvard.edu/29451055/
2 papers you can look at when thinking about feasibility and safety of short term abx treatment:
How Long study (was included in Cochrane review)
https://pubmed.ncbi.nlm.nih.gov/29153975/
ANTIBIOSTOP study …https://pubmed-ncbi-nlm-nih-gov.ezp-prod1.hul.harvard.edu/29451055/
13/
At the end of the day, the key to approaching F&N is individualizing your evaluation:
 What ppx prior to admission
What ppx prior to admission
 Patient clinical status
Patient clinical status
 New medications
New medications
 Expected duration of neutropenia
Expected duration of neutropenia
 Next chemotherapy scheduled
Next chemotherapy scheduled
 Timing of infection risk
Timing of infection risk
At the end of the day, the key to approaching F&N is individualizing your evaluation:
 What ppx prior to admission
What ppx prior to admission Patient clinical status
Patient clinical status New medications
New medications Expected duration of neutropenia
Expected duration of neutropenia Next chemotherapy scheduled
Next chemotherapy scheduled Timing of infection risk
Timing of infection risk
14/
IDSA GL: https://academic.oup.com/cid/article/52/4/e56/382256
NCCN GL: http://NCCN.org
ECIL GL: https://pubmed.ncbi.nlm.nih.gov/24323983/
IDSA GL: https://academic.oup.com/cid/article/52/4/e56/382256
NCCN GL: http://NCCN.org
ECIL GL: https://pubmed.ncbi.nlm.nih.gov/24323983/
Today's #IDFellows #Tweetorial is brought to you by @swinndong from @BIDMC_IDFellows!
@wuIDq @IUIDfellowship @UAB_ID @yaleIDfellows @templeID1 @VUMC_IC @MayoclinicINFD @MGH_ID @MontefioreID @UNMC_ID @UVA_ID @OhioState_ID @UTSWinfDis @BrownIDprogram @RushCCH_ID @OHSU_ID
@wuIDq @IUIDfellowship @UAB_ID @yaleIDfellows @templeID1 @VUMC_IC @MayoclinicINFD @MGH_ID @MontefioreID @UNMC_ID @UVA_ID @OhioState_ID @UTSWinfDis @BrownIDprogram @RushCCH_ID @OHSU_ID

 Read on Twitter
Read on Twitter