Proud to present our follow up data on our COVID-19 DISCOVER cohort here in @ResearchNBT @NorthBristolNHS @BristolARU . Important implications for #LongCovid, follow up, and policy makers ( @BTSrespiratory).
https://www.medrxiv.org/content/10.1101/2020.08.12.20173526v1
https://www.medrxiv.org/content/10.1101/2020.08.12.20173526v1
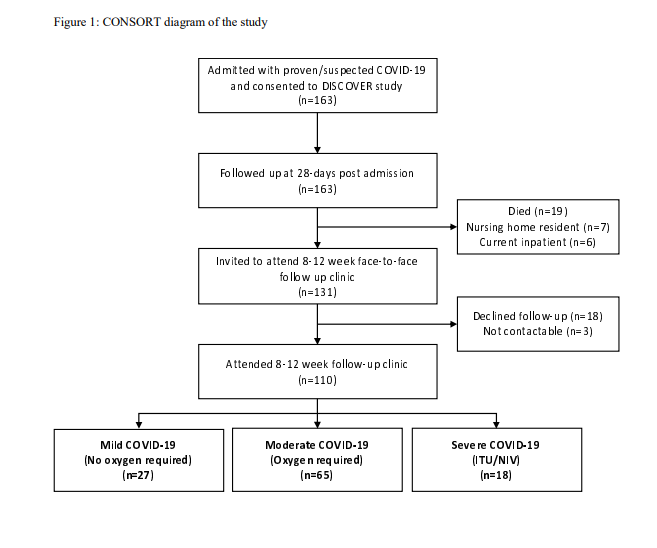
We prospectively recruited and followed up in-person patients with COVID-19 in Bristol, UK. Demographics and CONSORT diagram below. Nearly all agreed to attend. In clinic, we performed lung function, QoL scores, symptoms cores, and a CXR.
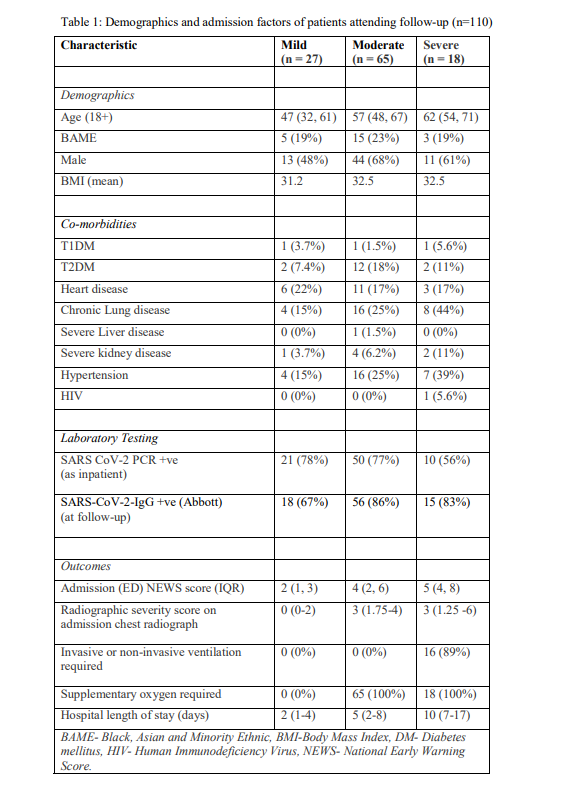
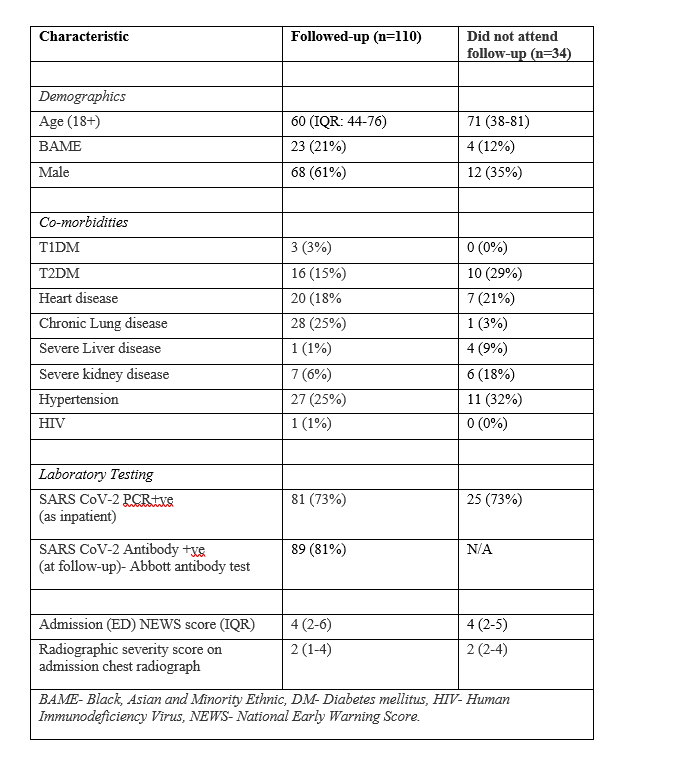
We then split patients by severity: mild = no 02, moderate = 02 only, severe = ITU/NIV. Unsurprisingly, severe patients were older and had more commodities. Those we followed up were not markedly different from those that attended. Median time to f/u 83 days (IQR 74-88 days).
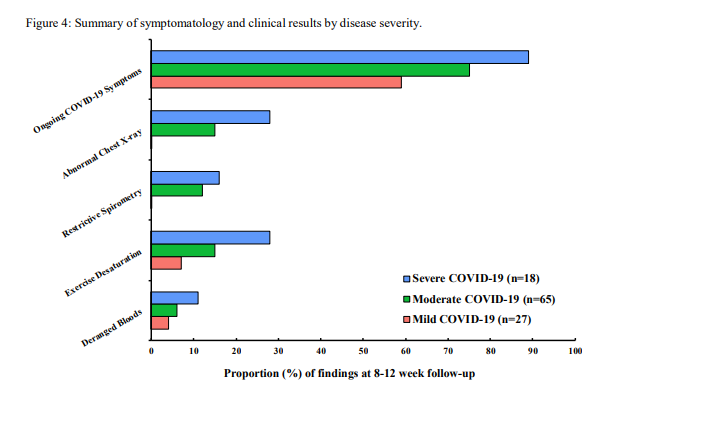
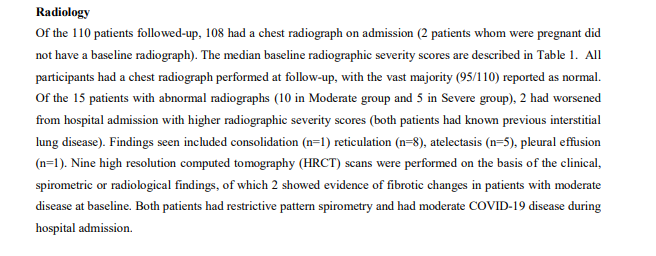
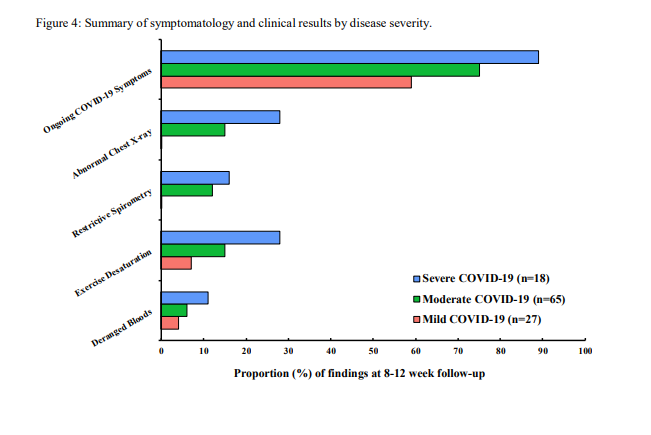
Radiology: Surprisingly, radiological abnormalities were rare, and most were in patients with pre-existing lung disease. 2 patients had HRCT that showed fibrosis. Importantly no patient with mild disease (no 02) had an abnormal CXR. This has useful implications for f/u!
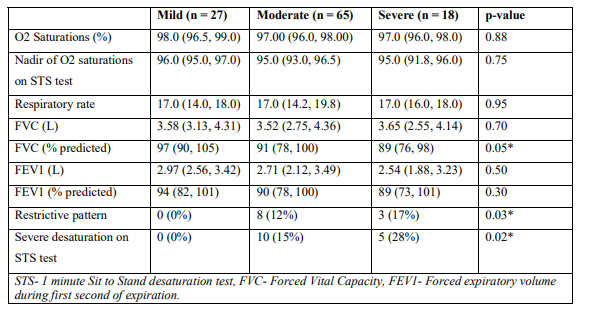
Lung function: Unsurprisingly, lung function was worse in severe disease, but actually, lung function was pretty normal in many patients in mild/moderate disease. Again, no patient with mild disease had significantly abnormal spirometry.
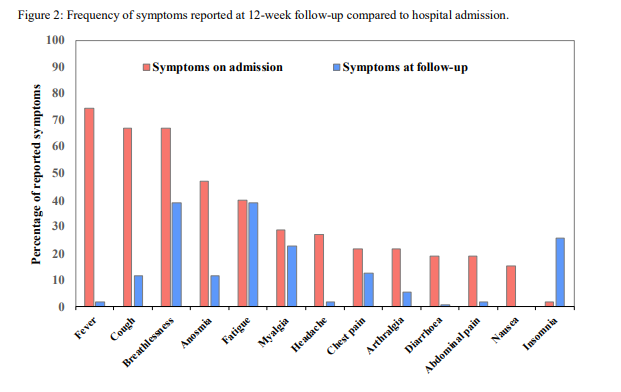
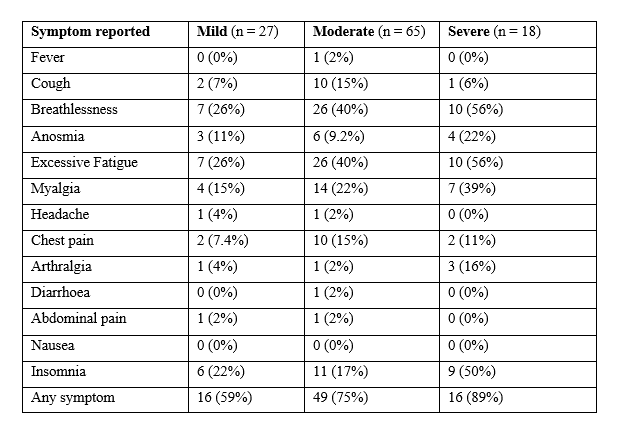
Symptoms: Unlike radiology/lung function - symptoms were VERY common across all severities of COVID-19 - this is #LongCovid. 74% of patients had >=1 symptom at follow up. Breathlessness, insomnia, and excessive fatigue were very common.
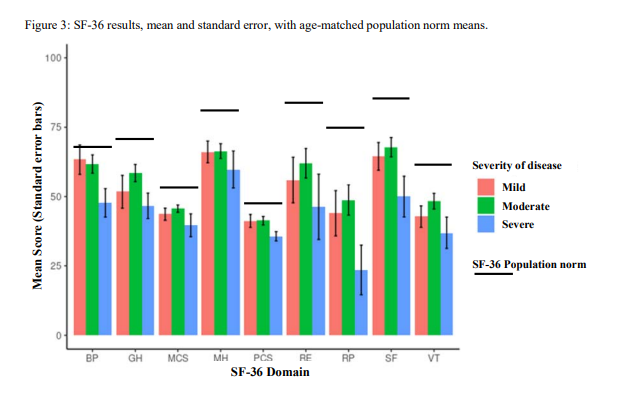
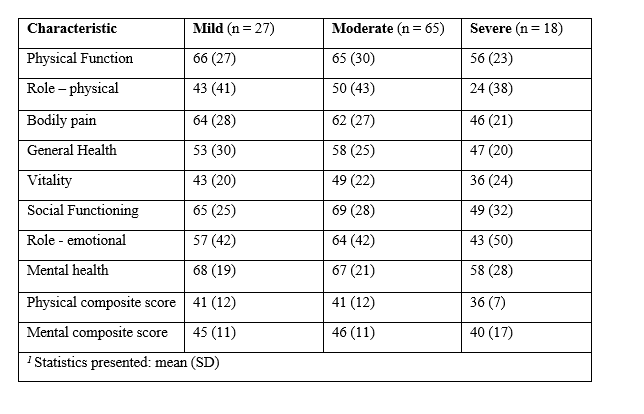
QoL: We performed SF-36, a validated QoL score on all patients. We noted marked deficits (particularly in physical function) compared to age-adjusted population norms.
(Of note - comparisons are hard - this is a similar QoL to many pneumonia cohorts - see attached - but QoL is strongly associated with age and these patients are very young compared to pneumonia patients)
http://dx.doi.org/10.1086/317495
http://dx.doi.org/10.1378/chest.130.4.1165 http://dx.doi.org/10.1186/s12955-018-0854-6
http://dx.doi.org/10.1086/317495
http://dx.doi.org/10.1378/chest.130.4.1165 http://dx.doi.org/10.1186/s12955-018-0854-6
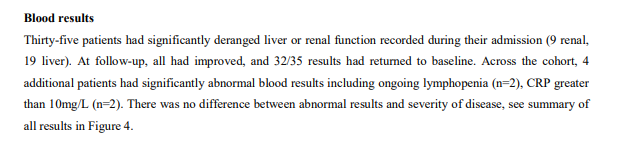
Bloods: (we looked at initial bloods in a previous paper - https://www.medrxiv.org/content/10.1101/2020.06.25.20137935v1). However, reassuringly, 'routine' blood abnormalities were rare in this cohort. Perhaps unnecessary in f/u?
Summary: Reduced QoL and symptoms very common at around 3 months in COVID-19. However, reassuringly, CXR and lung function findings are reassuring (particularly in patients who never required oxygen). Implications?
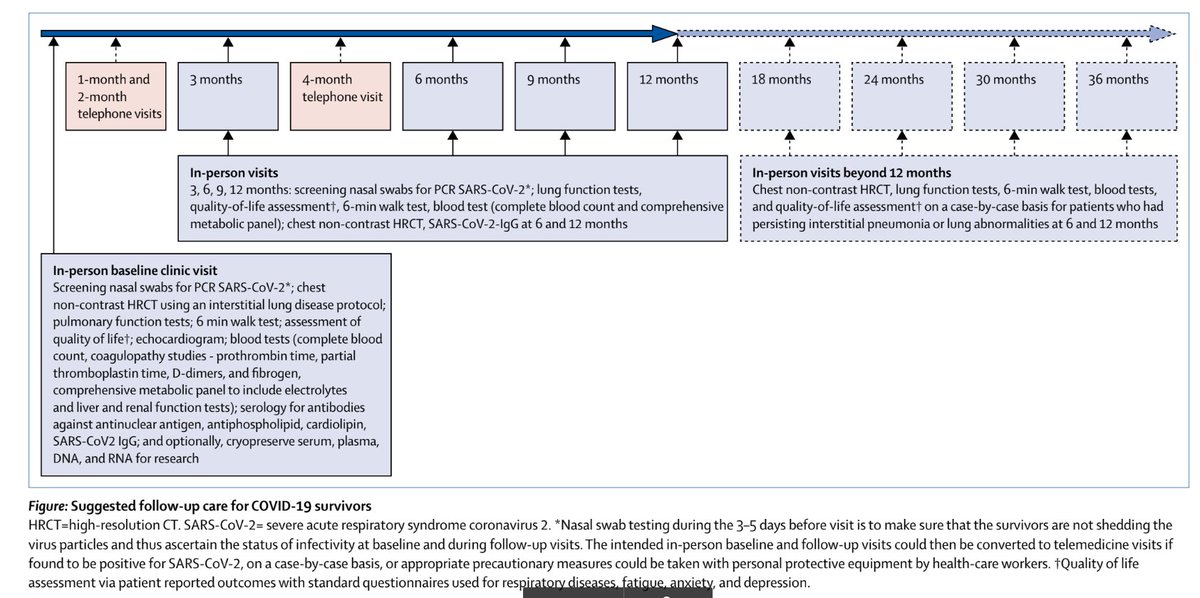
Many bodies/people have proposed f/u strategies: e.g. @BTSrespiratory ( https://www.brit-thoracic.org.uk/about-us/covid-19-information-for-the-respiratory-community/) or this (rather excessive) figure from https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30349-0/fulltext or https://www.bmj.com/content/370/bmj.m3001
And just 5 days ago from @trishgreenhalgh
https://www.bmj.com/content/370/bmj.m3026. However, what we don't know - is whether these tests will help people - or improve outcomes (cc @drjessicawatson @mgtmccartney).
https://www.bmj.com/content/370/bmj.m3026. However, what we don't know - is whether these tests will help people - or improve outcomes (cc @drjessicawatson @mgtmccartney).
This (small) study shows that clinical (radiographic, spirometric, blood) abnormalities are rare (well, non-existent!) in mild (no oxygen requirement) COVID-19, and infrequent in moderate disease. However..
QoL and symptom burden are massive ( #LongCovid ). We need effective strategies to manage these impacts of COVID-19 - on people - perhaps rather than performing lots of testing on patients who have had mild COVID-19.
Many thanks to @DavidT_Arnold @BristolARU @SuperSouthmead @BristolUncover @NorthBristolNHS @ResearchNBT @TheJollyHog (and all the clinicians, nurses, lung physiologists, etc who stayed late to see these patients in the evenings to get this work done)
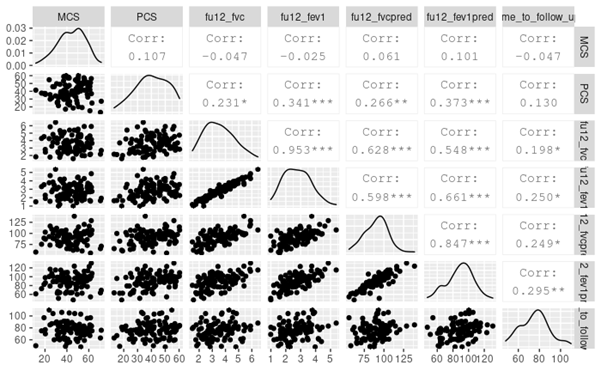
Bonus: We didn't include exploratory analyses in the work (I blame @DavidT_Arnold), but I include a scatter plot of the correlations between some of the lung function/time from follow up / QoL. There is a hint that: QoL is worse in those with severe disease, and
Symptoms and spirometry results seem to get better over time ... But numbers were a bit too small and we didn't have the time to include all the data and perform the appropriate analyses.

 Read on Twitter
Read on Twitter