As a #FPMRS #Urogyn fellow, several times a year, I get calls from the #ED & nurses on the floor to place bladder catheters for acute urinary retention in women, esp those w/ pelvic organ prolapse (POP). I'd love to share my tips n' tricks! A THREAD
to share my tips n' tricks! A THREAD  1/
1/
 to share my tips n' tricks! A THREAD
to share my tips n' tricks! A THREAD  1/
1/
STEP 1: Set yourself up for SUCCESS! 
- Anticipate the equipment (& help) that you'll need and have it ready by the bedside.
- Usually, this includes a bladder catheter kit (with antiseptic, lubrication, catheter, syringe, etc), good lighting, & an extra set of hands. 2/

- Anticipate the equipment (& help) that you'll need and have it ready by the bedside.
- Usually, this includes a bladder catheter kit (with antiseptic, lubrication, catheter, syringe, etc), good lighting, & an extra set of hands. 2/
STEP 2: Positioning is KEY
- If possible, position the patient in low lithotomy by placing her feet in stirrups.
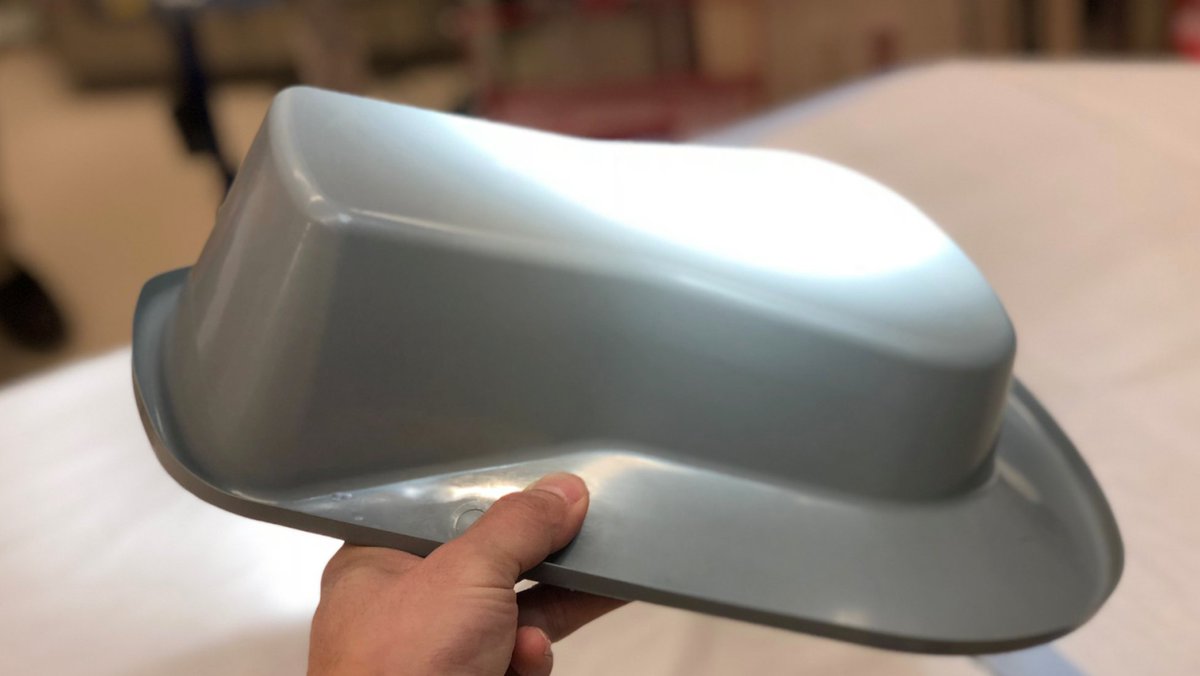
- If the bed does not have stirrups (or even if it does!), consider propping the patient's bottom on a flipped bedpan. https://bit.ly/2XYyqbl 3/

- If possible, position the patient in low lithotomy by placing her feet in stirrups.
- If the bed does not have stirrups (or even if it does!), consider propping the patient's bottom on a flipped bedpan. https://bit.ly/2XYyqbl 3/
STEP 2 (cont'd)
- Oftentimes, because of the patient's body habitus or the bed's mattress, the patient's dependent areas sink into the bed obscuring the view of her urethra.
 The bedpan trick is my FAVORITE & must be in your arsenal!!
The bedpan trick is my FAVORITE & must be in your arsenal!! 4/
4/
- Oftentimes, because of the patient's body habitus or the bed's mattress, the patient's dependent areas sink into the bed obscuring the view of her urethra.
 The bedpan trick is my FAVORITE & must be in your arsenal!!
The bedpan trick is my FAVORITE & must be in your arsenal!! 4/
4/
STEP 2 (cont'd)
- Don't forget to 1) ensure that the highest part of the flipped bedpan is facing caudad (vs cephalad) and 2) cover the bedpan with a soft towel for patient comfort.
- Utilize the "butterfly" or "frog-leg"
or "frog-leg"  position for increased exposure. 5/
position for increased exposure. 5/
- Don't forget to 1) ensure that the highest part of the flipped bedpan is facing caudad (vs cephalad) and 2) cover the bedpan with a soft towel for patient comfort.
- Utilize the "butterfly"
 or "frog-leg"
or "frog-leg"  position for increased exposure. 5/
position for increased exposure. 5/
STEP 3: SUCCESSFULLY placing the catheter 
- Use your non-dominate hand to retract the labial to expose the urethral meatus.
- If you can see the urethral opening, *congrats* the battle is half won! 6/
the urethral opening, *congrats* the battle is half won! 6/

- Use your non-dominate hand to retract the labial to expose the urethral meatus.
- If you can see
 the urethral opening, *congrats* the battle is half won! 6/
the urethral opening, *congrats* the battle is half won! 6/
STEP 3 (cont'd)
- If you can't see the urethra because of the patient's labia, ask your assistant to gently retract the labia for you. 7/
- If you can't see the urethra because of the patient's labia, ask your assistant to gently retract the labia for you. 7/
STEP 3 (cont'd)
- If you can't see the urethra because of POP:
 Reduce the prolapse w/ your hand or w/ an instrument like the vaginal speculum or sponge stick.
Reduce the prolapse w/ your hand or w/ an instrument like the vaginal speculum or sponge stick.
 If the POP won't reduce, try gently pushing down on the prolapse near the urethra until you see the urethra. 8/
If the POP won't reduce, try gently pushing down on the prolapse near the urethra until you see the urethra. 8/
- If you can't see the urethra because of POP:
 Reduce the prolapse w/ your hand or w/ an instrument like the vaginal speculum or sponge stick.
Reduce the prolapse w/ your hand or w/ an instrument like the vaginal speculum or sponge stick.  If the POP won't reduce, try gently pushing down on the prolapse near the urethra until you see the urethra. 8/
If the POP won't reduce, try gently pushing down on the prolapse near the urethra until you see the urethra. 8/
STEP 3 (cont'd)
- Place the lubricated end of the catheter tip into the urethra.
- Often times, the bladder will drain and the problem is solved!
- However, sometimes you'll meet resistance because the urethra is kinked from the POP 9/
9/
- Place the lubricated end of the catheter tip into the urethra.
- Often times, the bladder will drain and the problem is solved!
- However, sometimes you'll meet resistance because the urethra is kinked from the POP
 9/
9/
STEP 3 (cont'd)
- When this happens, don't advance the catheter but DO keep it in place while placing a finger in the vagina to gently support and straighten the urethra.
- Once the urethra is straightened, the bladder will drain which will eventually allow you to advance 10/
which will eventually allow you to advance 10/
- When this happens, don't advance the catheter but DO keep it in place while placing a finger in the vagina to gently support and straighten the urethra.
- Once the urethra is straightened, the bladder will drain
 which will eventually allow you to advance 10/
which will eventually allow you to advance 10/
STEP 3 (cont'd)
the catheter and/or further reduce the POP!
STEP 4: If all fails, call your #FPMRS #OBGYN #Urology friends! We're happy to help!
That's all I've got! Any other tips @SappenfieldMD @_sarahesteele @CassandraKisby @kmenhaji_md @iaddis @RRGonzalezMD @laurensiff?
the catheter and/or further reduce the POP!
STEP 4: If all fails, call your #FPMRS #OBGYN #Urology friends! We're happy to help!
That's all I've got! Any other tips @SappenfieldMD @_sarahesteele @CassandraKisby @kmenhaji_md @iaddis @RRGonzalezMD @laurensiff?

 Read on Twitter
Read on Twitter