1/ Covid ( @UCSF) Chronicles, Day 135
UCSF Medical Grand rounds today, available here https://tinyurl.com/y2tpw3h4 . If there could be such a thing as a “classic” set of topics in a pandemic that’s only 6 months old, today was it: Updates in testing, treatments and vaccines.
UCSF Medical Grand rounds today, available here https://tinyurl.com/y2tpw3h4 . If there could be such a thing as a “classic” set of topics in a pandemic that’s only 6 months old, today was it: Updates in testing, treatments and vaccines.
2/ Very brief local updates today to save room for grand rounds:
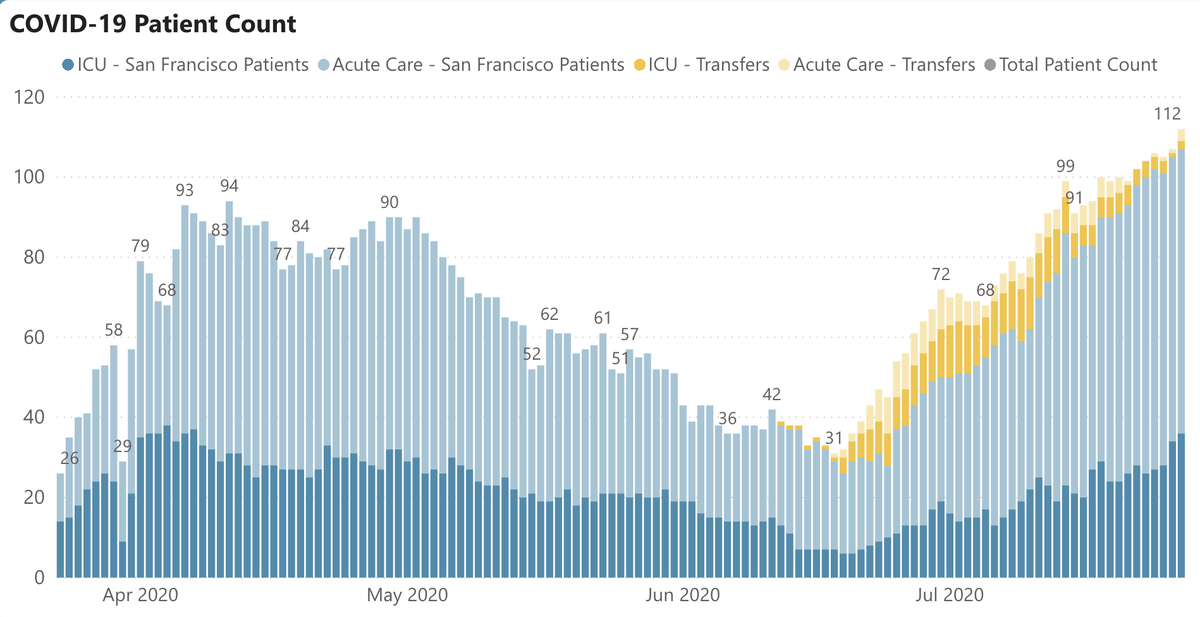
@UCSFHospitals, 35 pts, 9 vents. Possibly plateaued but significantly up over last few weeks (Fig L). SF hospitalizations also up, 112 today (R). Deaths still just 58 since March.
@UCSFHospitals, 35 pts, 9 vents. Possibly plateaued but significantly up over last few weeks (Fig L). SF hospitalizations also up, 112 today (R). Deaths still just 58 since March.
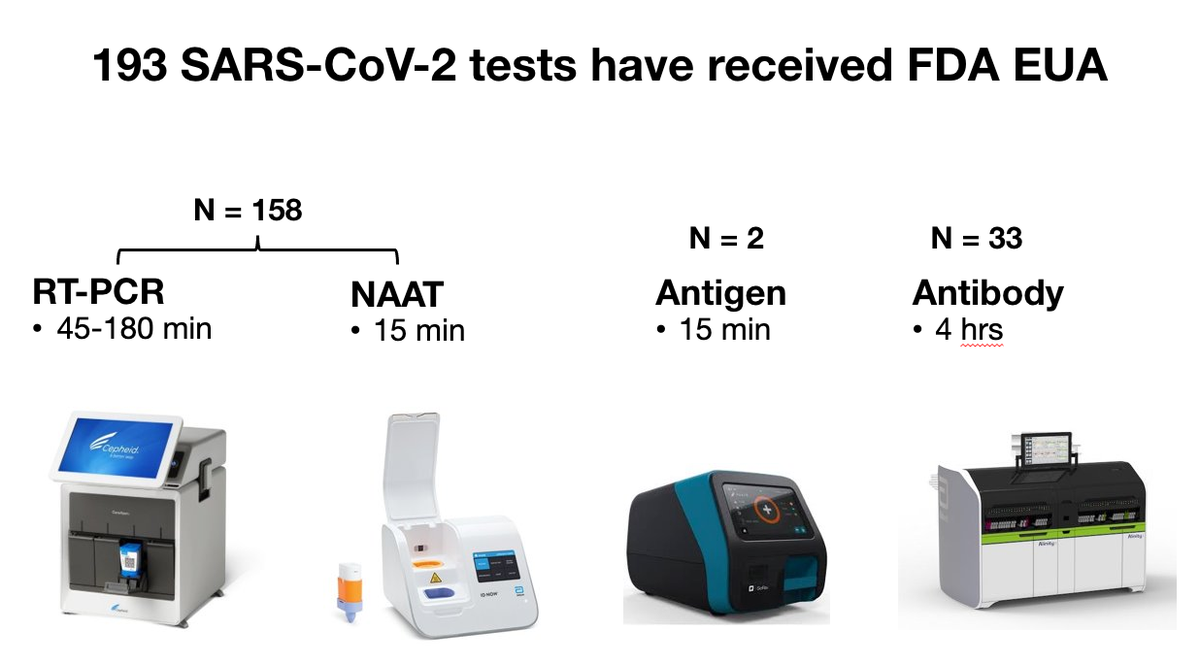
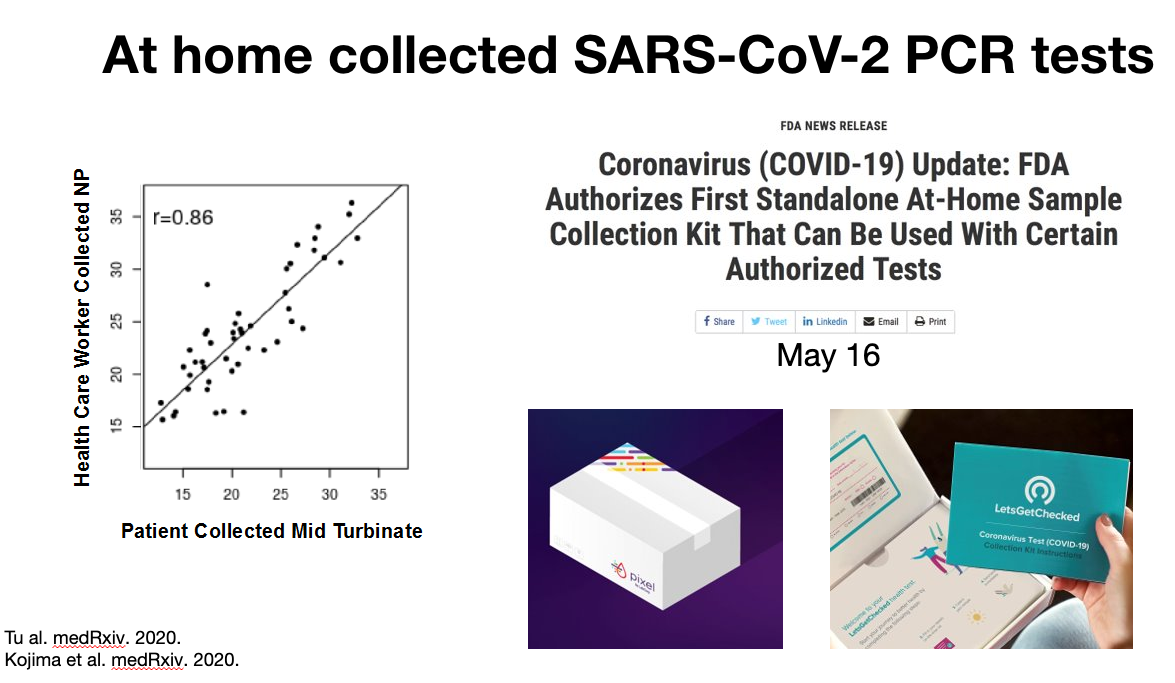
3/ Grand rounds. First, Chaz Langelier on testing. @ 7:00, 193 Covid tests approved by @US_FDA (Fig on L), incl. at-home tests: you swab your own nose (studies show it's as good as fancier deep swab), send it off, & get a result, hopefully (but not always) in few days (Fig R).
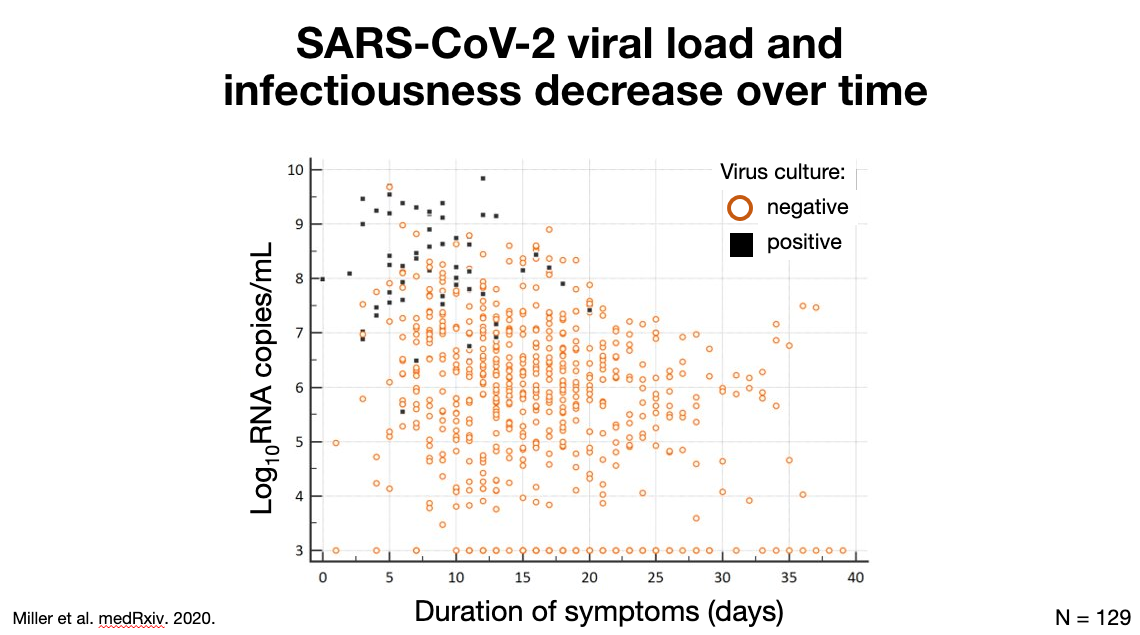
4/ @ 9:50, test timing matters. Fig L: association between day of infection & test positivity (viral & antibody). Viral load falls over time, as does test sensitivity. While PCR remains positive for a while, viral cultures (correlates w/ live virus) become neg by ~2 wks (Fig R).
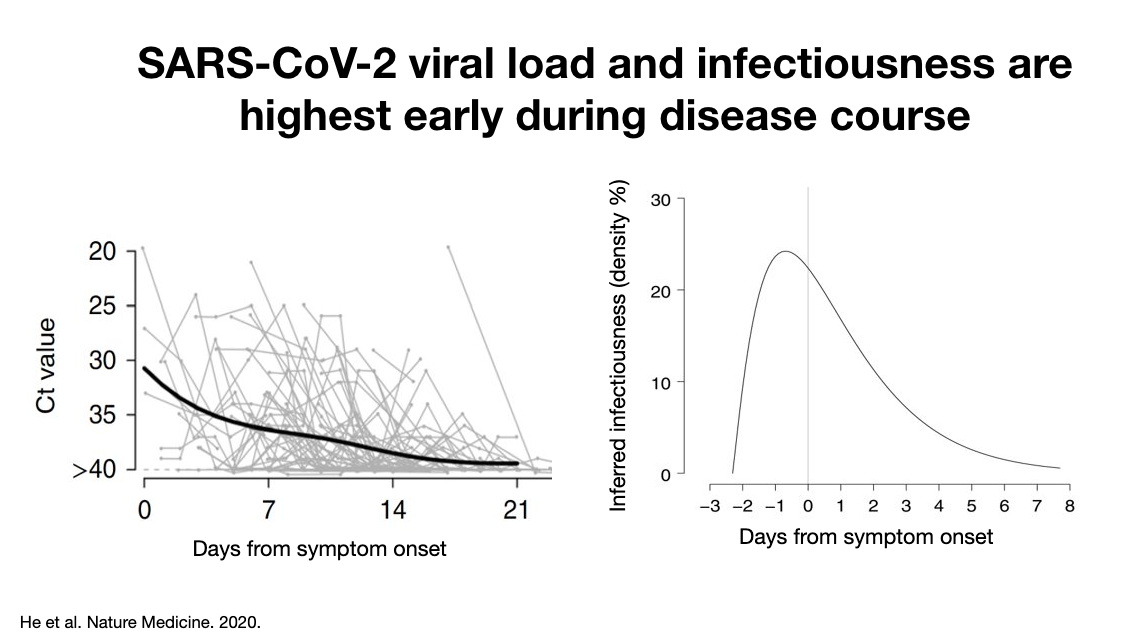
5/ @ 14:00, graph on left shows that Ct value (measure of infectiousness) is high in first days, then falls. Graph on R shows that patients are actually most infectious in the 1-2 days BEFORE they have symptoms; infectiousness falls off quickly after 2-3 days of symptoms.
6/ @ 16:00, newer thinking re: tests: perhaps better to focus on rapid tests (vs super-sensitive PCR tests). Rapids are less sensitive but may be good enough to detect infectious pts. Tradeoff of deploying more/cheaper tests may be net +: might miss a few cases, but few spreaders
7/ @ 20:30, so when do we require a very sensitive test? High risk settings, hospitalized pts: yes. But in the community, Chaz argues that widespread use of faster, less sensitive tests might do more to decrease transmission than limiting ourselves to slower, PCR-based tests.
8/ @ 18:30 Test turnaround matters too. Study demonstrated that daily use of quick but less sensitive test would lower Ro a lot. If you test less frequently, doesn't help decrease transmission as much. Once you're @ 1-2 wk turnaround times, does very little to lower transmission.
9/ @ 21:20, on pooled testing: reasonable if prevalence very low (<~5%; note that CA is ~7.5%) since you’ll won't have many +'s to follow-up. But once prevalence is >5%, not cost effective, since you’ll spend more time retesting samples than doing individual tests in first place.
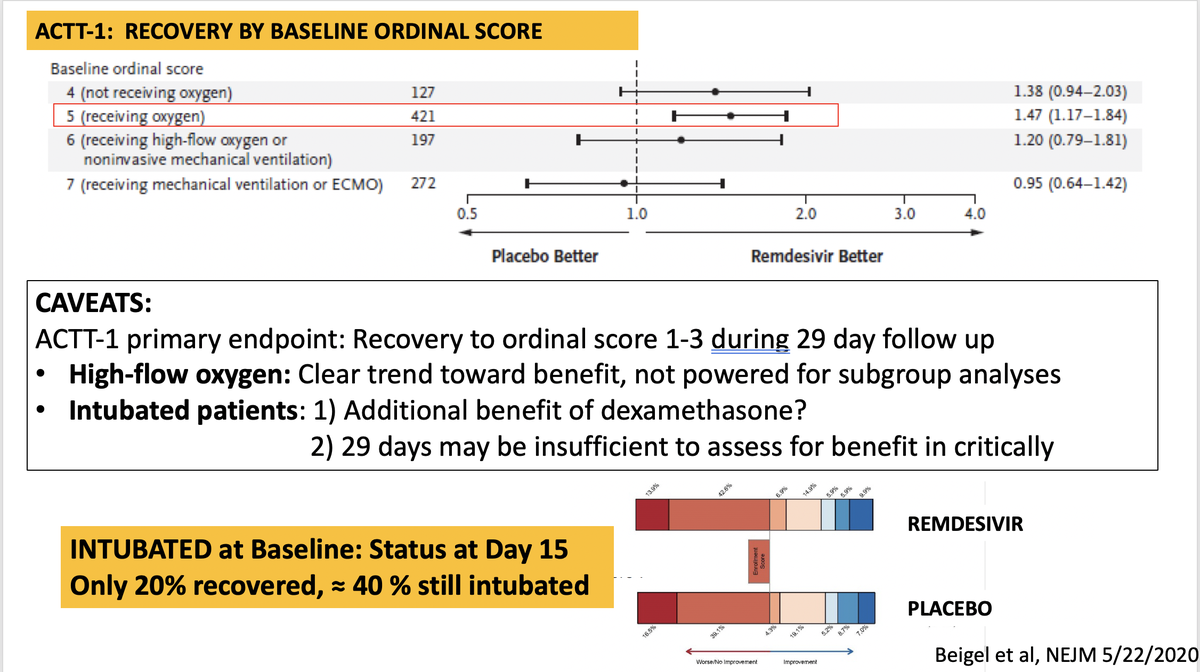
10/ Next, @annieluet on therapies. @ 28:30, NIH guidelines on Remdesivir use: prioritize RDV for pts on supplemental O2, over pts on high flow O2 or intubated. Annie reviews data: yes, more benefit for less sick pts, but underpowered in hi-flow O2, ICU. May be benefit there too.
11/ @ 35:30: Annie on dexamethasone. Benefit seen in ICU pts (41%→29% mortality). Pts who are hypoxic but out of ICU: real but small benefit. Patients not on O2: no benefit, and maybe even some worsening. So don't start steroids too early (such as in floor pt off O2 or outpt).
12/ @ 40:00: Exciting preliminary data on inhaled interferon beta. In study out via press release, Synairgen's interferon resulted in 79%↓ in intubation/death. “Intriguing” but need to see actual study. Other studies ongoing, incl. sub-q interferon & inhaled interferon at home.
13/ @ 44:00: Annie hoped we were done w/ hydroxychloroquine, but its in news again. 8 (!) randomized controlled studies: none found benefit; some possible harm. @ 1:19:30, she comments on Detroit study; far weaker study design than studies below. No indication for HCQ in Covid.
14/ @ 45:30: Outpatient therapy is “the next frontier.” Multiple promising approaches listed below, none proven. Would be great to prevent deterioration & spread. @ 1:17:30: we may give an outpt med only to high-risk pts; depends on how expensive & risky the meds turn out to be.
15/ @ 48:30: Convalescent plasma. Currently studying it @UCSF. In U.S., >50K pts have received it already. “While early signals look good, we don’t have randomized controlled data.” New meta-analysis does show mortality benefit. “Stay tuned for more info, but it looks promising.”
16/ @ 53:00: Joel Ernst on vaccines. Status report below. 3 vaccines have reported from Phase 1/2 trials, all showed neutralizing antibody production w/ acceptable side effects. Several different vaccine types; each w/ plusses & minuses. Also seeing T-cell responses in early data
17/ @ 57:45: Also promising: two published mice studies show transferring neutralizing antibodies induced by vaccination from one mice to another reduced the viral load. Shows that “neutralizing antibodies are actually a mechanism of protection, not just a phenomenon.”
18/ @ 1:00:35: Joel addresses studies showing waning antibodies over time. He’s not very concerned – “this is back to Immunology 101.” We have memory B cells that respond to infection by waking up when they see their pathogen. “I would not use this data as source of pessimism.”
19/ @ 1:04:30, how to test efficacy of vaccines. It may take >1yr to learn if vaccines work via nl trials; he describes benefits/drawbacks of human challenge trials (Fig). “There’s no precedent for doing challenge trials in infection that lacks reliable treatment.” Tricky stuff!
20/ @ 1:10:30: To finish talk, Joel discusses other challenging issues, including who should get vaccines first (Fig on L), and fact that 50% of Americans say they might not take an approved vaccine (Fig R). We need a new approach to public outreach and marketing.
21/ Starting at 1:12:30, a free-wheeling Q&A, including: 1) When is the earliest we'll know a vaccine works (Joel: “pretty unrealistic” that we’ll know at end of 2020); 2) Whether proving that a vaccine works in a 25 year old proves it’ll also work in 75 yo (Joel: probably so)…
22/ … 3) Have there been any re-infections? (Chaz: no definitive evidence; “cases” may be new non-Covid case w/ persistent PCR + from 1st infection); 4) What happened to saliva for viral testing? (Chaz: hasn’t gained traction, though it works just as well as swab)…
23/ Finally, @ 1:25:45, I asked all 3 when we’ll have a game-changing strategy that gets us to normal life, and what it would be: meds, vaccine, testing. All three say a year from now; only Joel thinks it’ll be with a vaccine. Chaz: testing. Annie, surprisingly, agrees: testing.
24/ Another superb and eye-opening session. Hope you have a chance to watch it (90 minutes). Again, it’s here: https://tinyurl.com/y2tpw3h4
Back tomorrow with some thoughts about San Francisco’s Covid performance, surge and all. Till then, stay safe.
Back tomorrow with some thoughts about San Francisco’s Covid performance, surge and all. Till then, stay safe.

 Read on Twitter
Read on Twitter