This is the third and last addition to my #MSPathJournalReview on #ihcpath from Dr. Bellizzi's @IHC_guy amazing paper:
"An Algorithmic Immunohistochemical Approach to Define Tumor Type and Assign Site of Origin"
"An Algorithmic Immunohistochemical Approach to Define Tumor Type and Assign Site of Origin"
For part two refer to: https://twitter.com/anueru432/status/1284094142755123200?s=19
So what's in store for us today?
-Site Specific Considerations
-Squamous cell vs Urothelial CA
-Approach to Neuroendocrine Neoplasms
And we'll end off with Triple Negative Malignant Neoplasms
#MSPathJournalReview
So what's in store for us today?
-Site Specific Considerations
-Squamous cell vs Urothelial CA
-Approach to Neuroendocrine Neoplasms
And we'll end off with Triple Negative Malignant Neoplasms
#MSPathJournalReview
To start off, a reminder:
 #ihcpath should be ancillary and only supportive, your main basis for diagnosis should come from a good patient history and good differentials from the H & E slide
#ihcpath should be ancillary and only supportive, your main basis for diagnosis should come from a good patient history and good differentials from the H & E slide
From Dr. Bellizzi: Use the fewest moves possible! https://twitter.com/IHC_guy/status/1286674988930674693?s=19
 #ihcpath should be ancillary and only supportive, your main basis for diagnosis should come from a good patient history and good differentials from the H & E slide
#ihcpath should be ancillary and only supportive, your main basis for diagnosis should come from a good patient history and good differentials from the H & E slideFrom Dr. Bellizzi: Use the fewest moves possible! https://twitter.com/IHC_guy/status/1286674988930674693?s=19
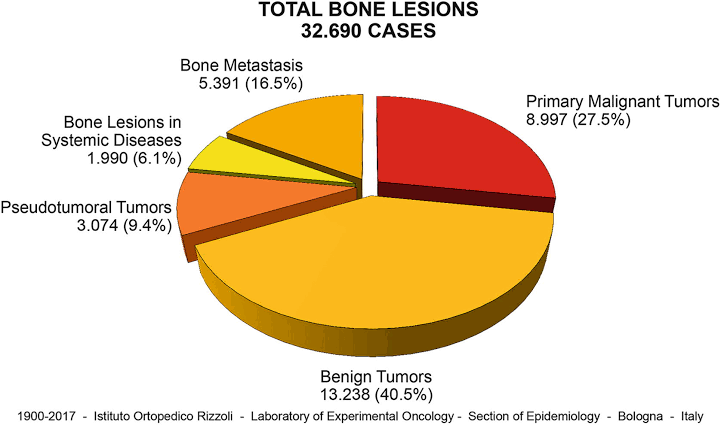
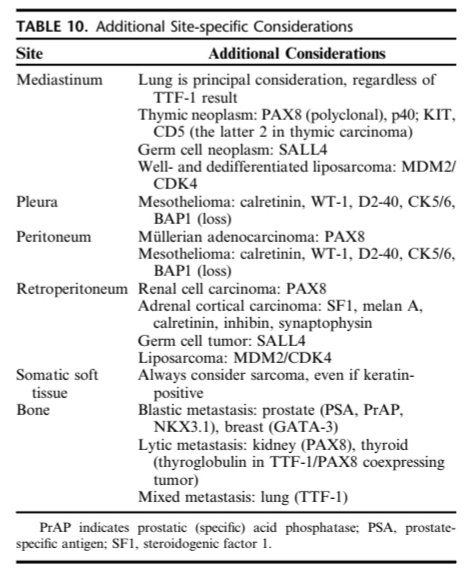
At any site, tumors primary to that site should be included in the ddx. Also, consider special predilection for metastasis to certain sites.
Such that primary considerations for a bone tumor should be:
1. A tumor of primary bone origin
2. Tumors with preferential bone mets
Such that primary considerations for a bone tumor should be:
1. A tumor of primary bone origin
2. Tumors with preferential bone mets
In the mediastinum,
Lung is primary consideration REGARDLESS of TTF-1 result
(As highlighted by Dr. Mukhopadhyay @smlungpathguy : https://twitter.com/smlungpathguy/status/1269744969411178500?s=19)
Other considerations include thymic neoplasm, GCT, and well and dediff. liposarcoma.
Lung is primary consideration REGARDLESS of TTF-1 result
(As highlighted by Dr. Mukhopadhyay @smlungpathguy : https://twitter.com/smlungpathguy/status/1269744969411178500?s=19)
Other considerations include thymic neoplasm, GCT, and well and dediff. liposarcoma.
In the body cavities- mesothelioma should always be a consideration
*for the peritoneum- add Müllerian AdenoCA in your ddx
In the retroperitoneum, consider the retroperitoneal organs- RCC, Adrenal Cortical CA, GCT (in fetal life at least ), liposarcoma
), liposarcoma
*for the peritoneum- add Müllerian AdenoCA in your ddx
In the retroperitoneum, consider the retroperitoneal organs- RCC, Adrenal Cortical CA, GCT (in fetal life at least
 ), liposarcoma
), liposarcoma
In the somatic soft tissue, sarcomas should be prime ddx
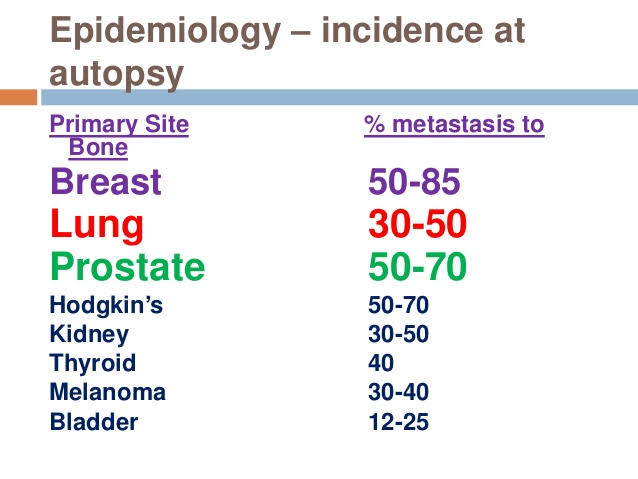
In the bone, remember imaging plays a huge role in dx:
Considering if the tumor is blastic or lytic would favor certain diagnoses...
Mets are also more common than primaries
Breast, lung, and prostate are most common
In the bone, remember imaging plays a huge role in dx:
Considering if the tumor is blastic or lytic would favor certain diagnoses...
Mets are also more common than primaries
Breast, lung, and prostate are most common
Moving on...
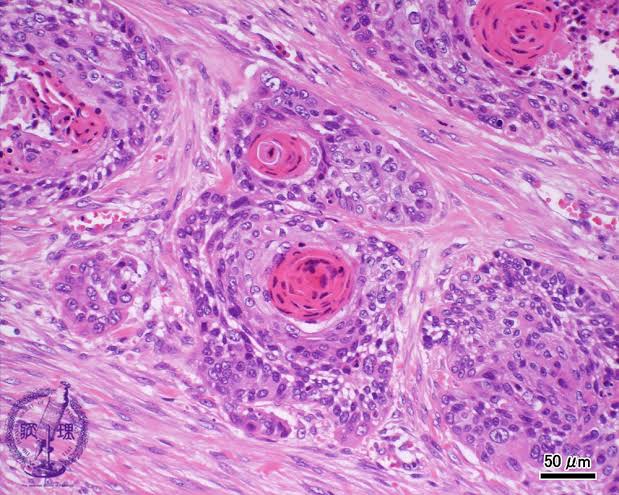
The difficulty in determining between a squamous and a urothelial origin stems from having similar morphologies in H & E.
Clues that may point toward SCC would be intercellular bridges and keratin pearl formation, however challenge is in less differentiated tumors.
The difficulty in determining between a squamous and a urothelial origin stems from having similar morphologies in H & E.
Clues that may point toward SCC would be intercellular bridges and keratin pearl formation, however challenge is in less differentiated tumors.
Such as in this case: (from Dr. Bratu, Romanian Journal of Morphology and Embryology, 2015)
No keratin pearl formation
Intercellular bridges aren't too evident

Here is where IHC can help.
No keratin pearl formation
Intercellular bridges aren't too evident


Here is where IHC can help.
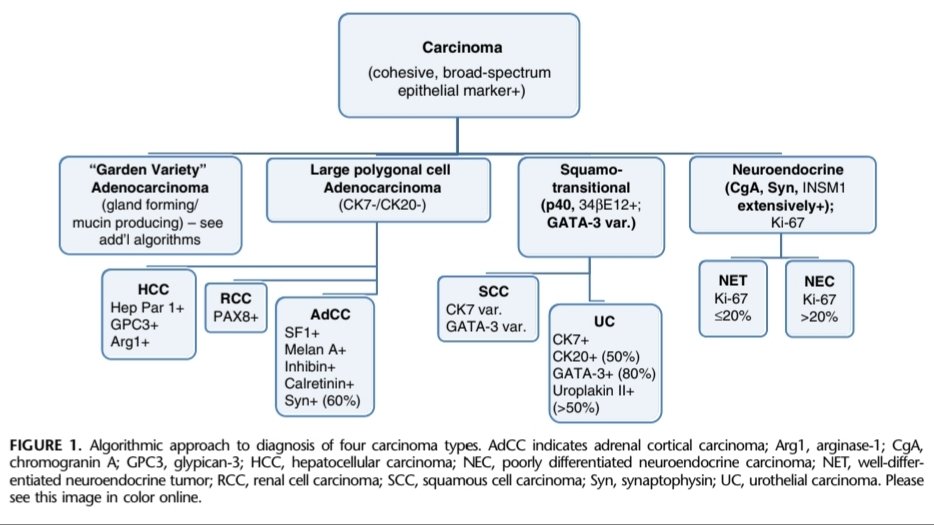
Once determining a carcinoma from the H & E slide and atleast 1 broad spectrum keratin,
Confirm a squamotransitional origin by p40, 34BE12, and GATA-3.
Though if one were to choose only 1, go with p40- sensitive for BOTH squamous and transitional.
(Focus on the third arm )
)
Confirm a squamotransitional origin by p40, 34BE12, and GATA-3.
Though if one were to choose only 1, go with p40- sensitive for BOTH squamous and transitional.
(Focus on the third arm
 )
)
Markers favoring urothelial:
1. GATA-3: however it is also expressed SCCs of cutaneous or genitourinary origin BUT in a weak or patchy manner
2. CK20 is highly specific for but only +ve in 54% of UC
3. Uroplakin II is specific and sensitive https://twitter.com/kis_lorand/status/1122986084563083264?s=19
1. GATA-3: however it is also expressed SCCs of cutaneous or genitourinary origin BUT in a weak or patchy manner
2. CK20 is highly specific for but only +ve in 54% of UC
3. Uroplakin II is specific and sensitive https://twitter.com/kis_lorand/status/1122986084563083264?s=19
To support on Uroplakin II's sensitivity and specificity- Dr. Sangoi's review: https://twitter.com/slusagar/status/1120703126145605633?s=19
In the halfway mark!  So here's what we learned so far!
So here's what we learned so far!
 Differential diagnoses can be narrowed down based on the site of the tumor
Differential diagnoses can be narrowed down based on the site of the tumor
 Consider a squamotransitional origin in a CA with p40 and/or 34BE12 positivity
Consider a squamotransitional origin in a CA with p40 and/or 34BE12 positivity
 GATA-3, CK20, Uroplakin II serve to favor urothelial CA
GATA-3, CK20, Uroplakin II serve to favor urothelial CA
 So here's what we learned so far!
So here's what we learned so far! Differential diagnoses can be narrowed down based on the site of the tumor
Differential diagnoses can be narrowed down based on the site of the tumor  Consider a squamotransitional origin in a CA with p40 and/or 34BE12 positivity
Consider a squamotransitional origin in a CA with p40 and/or 34BE12 positivity GATA-3, CK20, Uroplakin II serve to favor urothelial CA
GATA-3, CK20, Uroplakin II serve to favor urothelial CA
Congratulations! And to take a break on the pinks and purples, here's a view from a boat ride in one of the islands here in the Philippines 
 I wish #pathtwitter can come and visit once COVID's away and gone
I wish #pathtwitter can come and visit once COVID's away and gone 

 I wish #pathtwitter can come and visit once COVID's away and gone
I wish #pathtwitter can come and visit once COVID's away and gone 
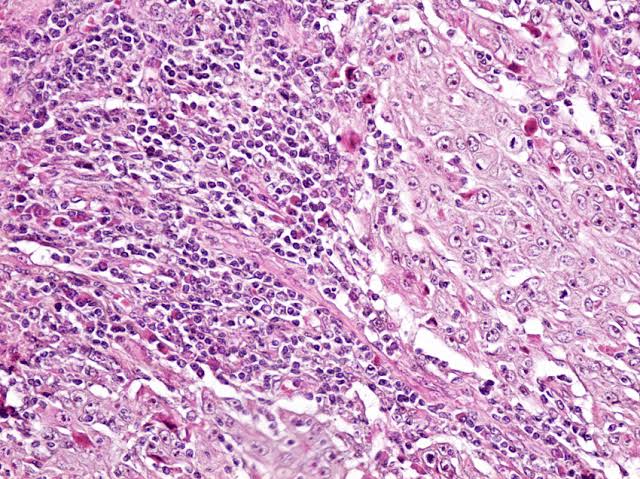
On towards Neuroendocrine Neoplasms!
They can be:
Well diff. NE tumors (WDNET)
Poorly diff. NE CA
(PDNEC)
Pheochromocytoma
Paragangliomas
The classic appearance for this would be round nuclei with salt and pepper chromatin- as exemplified here: https://twitter.com/yro854/status/1038877327231467520?s=19
They can be:
Well diff. NE tumors (WDNET)
Poorly diff. NE CA
(PDNEC)
Pheochromocytoma
Paragangliomas
The classic appearance for this would be round nuclei with salt and pepper chromatin- as exemplified here: https://twitter.com/yro854/status/1038877327231467520?s=19
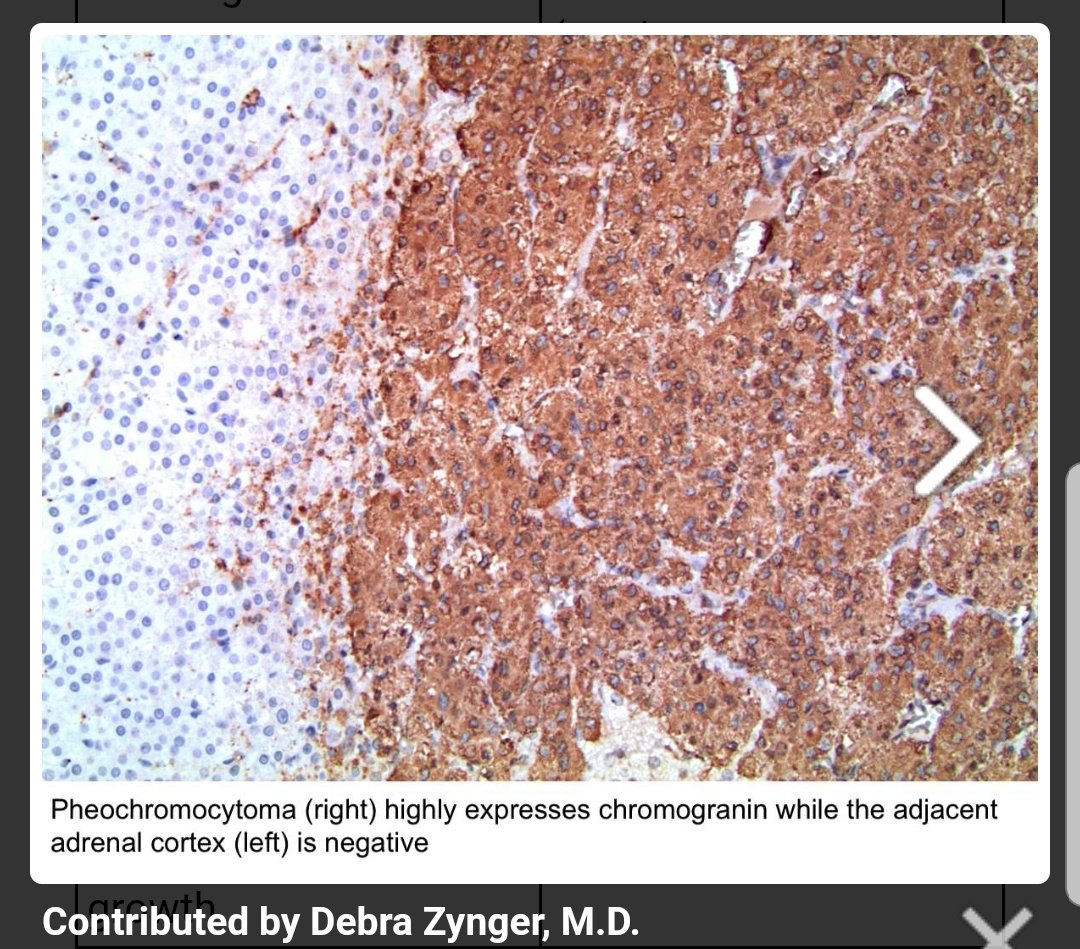
In general: WDNETs and PDNECs express broad spectrum epithelial markers, but Pheochromocytomas and Parangliomas DO NOT
Chromogranin A and Synaptophysin are considered the classic neuroendocrine markers;
between the two, CgA is more specific, while Syn is more sensitive.
Chromogranin A and Synaptophysin are considered the classic neuroendocrine markers;
between the two, CgA is more specific, while Syn is more sensitive.
WDNETs, pheo & paraG should ALWAYS express CgA.
1/4 of PDNECs do not express both Syn and CgA
In these cases, INSM1, dot-like keratin expression, & TTF1 positivity may serve as surrogate NE markers.
Aside from NE neoplasms, INSM1 will stain others... https://twitter.com/TheKarenPinto/status/1265416550686896129?s=19
1/4 of PDNECs do not express both Syn and CgA
In these cases, INSM1, dot-like keratin expression, & TTF1 positivity may serve as surrogate NE markers.
Aside from NE neoplasms, INSM1 will stain others... https://twitter.com/TheKarenPinto/status/1265416550686896129?s=19
However PROCEED WITH CAUTION, when using IHCs to determine NE origin.
OCCULT NEUROENDOCRINE DIFFERENTIATION- 10-20% of non-NE, non-small cell neoplasms from various anatomic sites will express 1 or more NE markers.
However expression is usually scattered and diffuse.
OCCULT NEUROENDOCRINE DIFFERENTIATION- 10-20% of non-NE, non-small cell neoplasms from various anatomic sites will express 1 or more NE markers.
However expression is usually scattered and diffuse.
Also never forget that the best IHCs are a good history and a skilled morphologist 
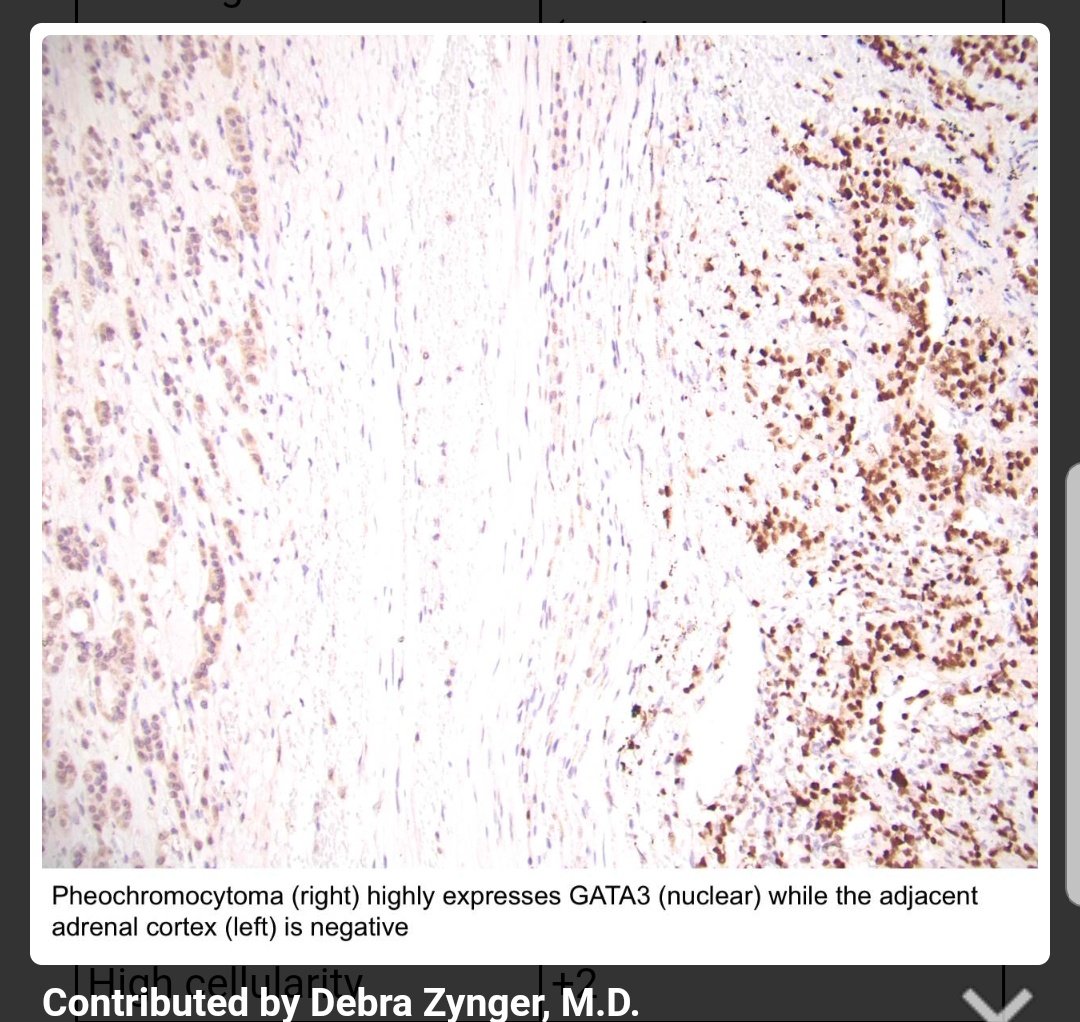
Keratin negativity is your major clue for a pheo/paraG origin.
To support this, there should be CgA and Syn positivity.
Other markers to support the diagnosis is GATA-3 and loss of SDHB.

Keratin negativity is your major clue for a pheo/paraG origin.
To support this, there should be CgA and Syn positivity.
Other markers to support the diagnosis is GATA-3 and loss of SDHB.
For Well Diff. NE tumors (WDNETs)
Determining the primary origin of the tumor would be important in management and prognosis.
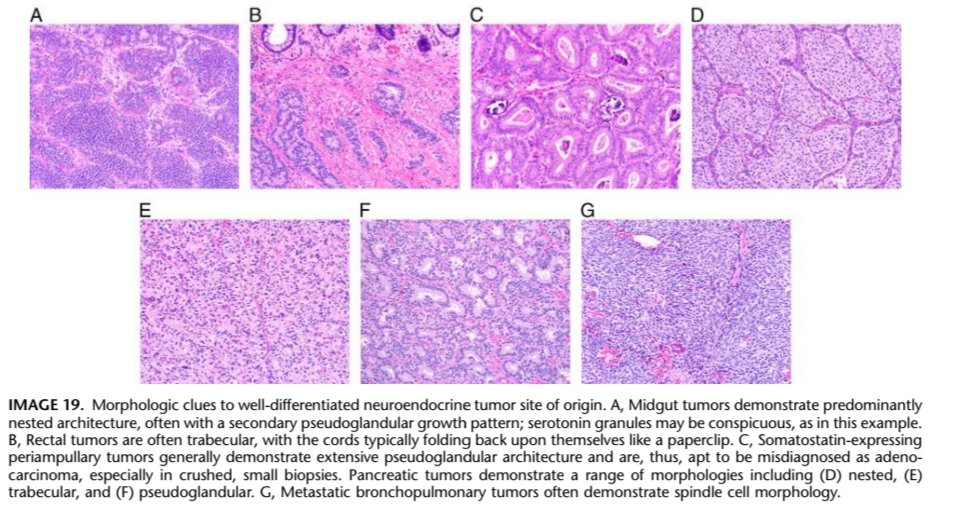
Morphology and architectural pattern play a role in dx:
Nested- midgut
Trabecular- rectal
Pseudoglandular- periampullary
Spindly- bronchopulmonary
Determining the primary origin of the tumor would be important in management and prognosis.
Morphology and architectural pattern play a role in dx:
Nested- midgut
Trabecular- rectal
Pseudoglandular- periampullary
Spindly- bronchopulmonary
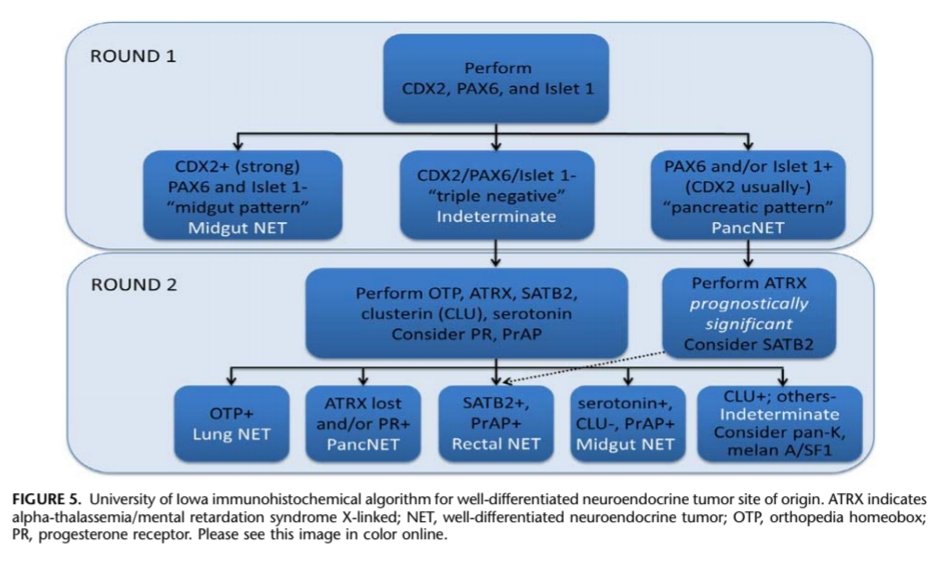
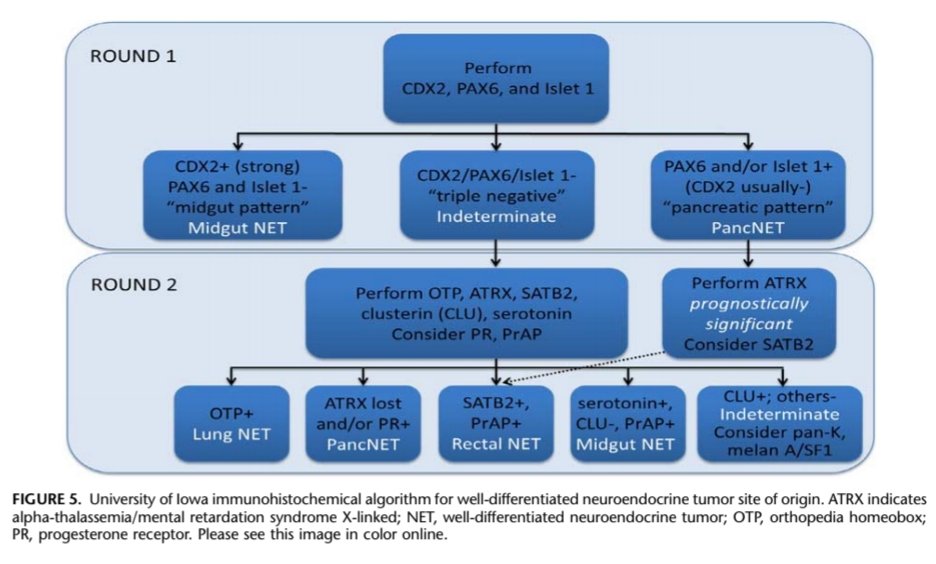
However an ihc algorithm can also be used in determining the primary, especially if imaging and history yields no lesions...
This algorithm is based on the fact that most occult primaries are pancreatic or jejunoileal in origin- as these are hard to see in imaging (endoscopy)
This algorithm is based on the fact that most occult primaries are pancreatic or jejunoileal in origin- as these are hard to see in imaging (endoscopy)
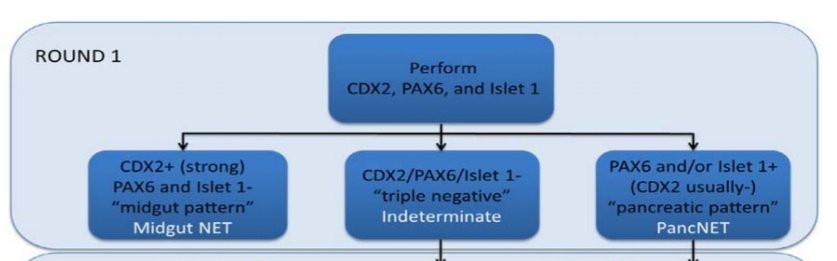
In the first round of IHCs, effort is made to rule these two out-
wherein a strong CDX2 staining with negative PAX6 or Islet1 points toward a Midgut NET
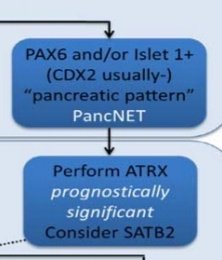
While positive PAX6 and/or Islet1 will point towards a PancNET.
Negative staining for these 3 would push towards Round 2.
wherein a strong CDX2 staining with negative PAX6 or Islet1 points toward a Midgut NET
While positive PAX6 and/or Islet1 will point towards a PancNET.
Negative staining for these 3 would push towards Round 2.
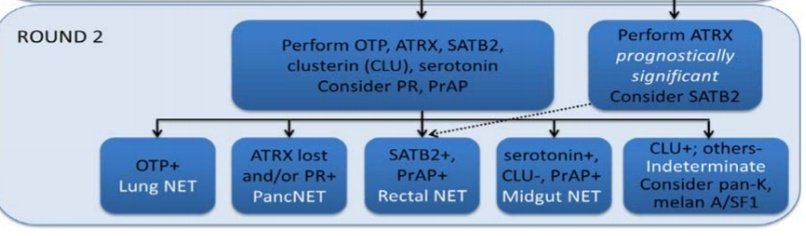
The second round will focus on other possible origins, while not ruling out the possibility of PancNET or midgut NET.
OTP+: lung
ATRX loss and/or PR +ve: pancreas
SATB2+, Prostatic Acid Phosphatase (PrAP) +: rectal
Serotonin+, clusterin -ve, PrAP+: Midgut
OTP+: lung
ATRX loss and/or PR +ve: pancreas
SATB2+, Prostatic Acid Phosphatase (PrAP) +: rectal
Serotonin+, clusterin -ve, PrAP+: Midgut
Also in Round 1, a diagnosis of PancNET can be confirmed with ATRX loss, or challenged by SATB2- wherein a positive stain would point towards rectal origin.
(My apologies to Dr. Bellizzi for cutting his algorithm in segments )
)
(My apologies to Dr. Bellizzi for cutting his algorithm in segments
 )
)
And as a perfect summary, return back to the whole picture 
(There's another "1-step" algorithm, but Ill challenge the readers to look for it in the paper )
)

(There's another "1-step" algorithm, but Ill challenge the readers to look for it in the paper
 )
)
However when we come to poorly diff. NE Carcinomas (PDNECs) there is limited utility of IHCs in assigning site of origin.
A notable exception is the use of CK20 positivity and neurofilament (NF) in diagnosis of Merkel Cell Carcinoma. https://twitter.com/SGottesmanMD/status/924042175117189120?s=19
A notable exception is the use of CK20 positivity and neurofilament (NF) in diagnosis of Merkel Cell Carcinoma. https://twitter.com/SGottesmanMD/status/924042175117189120?s=19
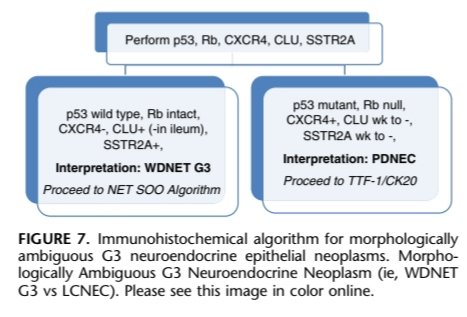
An area of controversy is the differentiation of WDNET G3 and PDNEC.
Ki67 cannot be used as a classifier since there is substantial overlap, but p53 mutant and Rb null phenotype would point toward a PDNEC.
Clusterin+ (except in WDNET of ileum) and SSTR2A+ point towards WDNET.
Ki67 cannot be used as a classifier since there is substantial overlap, but p53 mutant and Rb null phenotype would point toward a PDNEC.
Clusterin+ (except in WDNET of ileum) and SSTR2A+ point towards WDNET.
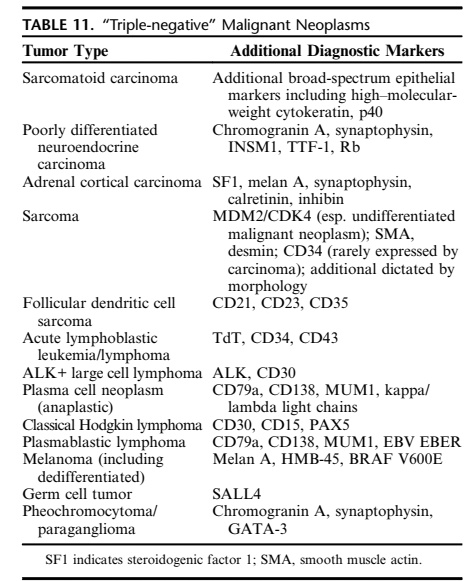
To end this #MSPathJournalReview of #ihcpath we ask the question
What about tumors which go blue (are negative) with keratins, CD45, and S100?
We call these Triple Negative Malignant Neoplasms.
What about tumors which go blue (are negative) with keratins, CD45, and S100?
We call these Triple Negative Malignant Neoplasms.
You consider
Keratin negative carcinomas
-Sarcomatoid CA, Adrenal Cortical Carcinomas
Sarcomas (since NO screening marker for sarcomas )
)
CD45 -ve lymphomas
-FDCS, ALK+ve large cell lymphoma, CHL, etc.
Rare s100 -ve melanoma
GCT (esp. Seminoma)
Pheo/ParaG!
Keratin negative carcinomas
-Sarcomatoid CA, Adrenal Cortical Carcinomas
Sarcomas (since NO screening marker for sarcomas
 )
)CD45 -ve lymphomas
-FDCS, ALK+ve large cell lymphoma, CHL, etc.
Rare s100 -ve melanoma
GCT (esp. Seminoma)
Pheo/ParaG!
To summarize the second part,
 NE neoplasms pose a diagnostic challenge especially if they are metastasis from a distant site
NE neoplasms pose a diagnostic challenge especially if they are metastasis from a distant site
 In WDNETs, IHCs can be utilized to know site of origin
In WDNETs, IHCs can be utilized to know site of origin
 IHCs can help determine bet. WDNET G3 and PDNECs
IHCs can help determine bet. WDNET G3 and PDNECs
 IHC panel can help in triple negatives
IHC panel can help in triple negatives
 NE neoplasms pose a diagnostic challenge especially if they are metastasis from a distant site
NE neoplasms pose a diagnostic challenge especially if they are metastasis from a distant site  In WDNETs, IHCs can be utilized to know site of origin
In WDNETs, IHCs can be utilized to know site of origin  IHCs can help determine bet. WDNET G3 and PDNECs
IHCs can help determine bet. WDNET G3 and PDNECs IHC panel can help in triple negatives
IHC panel can help in triple negatives
As something to consider, check out this case by Dr. Pijuan @lara_pijuan
For sure IHC was key in providing definitive diagnosis and management for the patient https://twitter.com/lara_pijuan/status/855151058838073345?s=19
https://twitter.com/lara_pijuan/status/855151058838073345?s=19
For sure IHC was key in providing definitive diagnosis and management for the patient
 https://twitter.com/lara_pijuan/status/855151058838073345?s=19
https://twitter.com/lara_pijuan/status/855151058838073345?s=19
I would again extend my appreciation to Dr. Bellizzi for the inspiration in #ihcpath, helping us all to love it one brown stain at a time 
A final disclaimer that I am open to corrections and suggestions. I am here to learn.
Tune in for the next #MSPathJournalReview

A final disclaimer that I am open to corrections and suggestions. I am here to learn.
Tune in for the next #MSPathJournalReview


 Read on Twitter
Read on Twitter