1/Listening today to @CDCgov Board of Scientific Counselors meeting that includes discussion of pain issues and a future opioid guideline...800-369-3110; participant 7563795 https://www.cdc.gov/injury/bsc/meetings.html
2/The 1st part focuses on opioid prescribing by specific dx, as published by Christina Mikosz, and boy this study's limitations stand out.... (also popularized by @BrianMannADK of NPR) https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2765703
3/Notably the study rides on a single diagnosis, not capturing any medical, social or life context comorbidities that normally should influence care decisions. It also doesn't portray if opioids were offered as 2nd, 3rd as opposed to 1st option
4/The Mikosz data relies on late 2016 to early 2017. Despite that following right after the CDC Guideline's release, she avows that "physician resistance" go Guidelines is a potential explanation. There is no Guideline that is fully absorbed and carried out instantly.
5/Again, any normal study of appropriate/inappropriateness of an Rx should ask about all clinical diagnoses in the patient, context, and what was tried before. This study captured none of the standard data- and yet it deduces that physicians are "resistant" to guidelines
6/The analysis central to CDC's discussion & was central to NPR's report lacked (a) race/ethnicity data (& therefore could not interrogate disparities in care); (b) comorbid medical or mental conditions; or (c) medical history. This was more limited than the average claims study
7/Commander Kinzie Lee of @CDCgov is speaking about stakeholder engagement for any future update to the CDC Guideline of 2016...
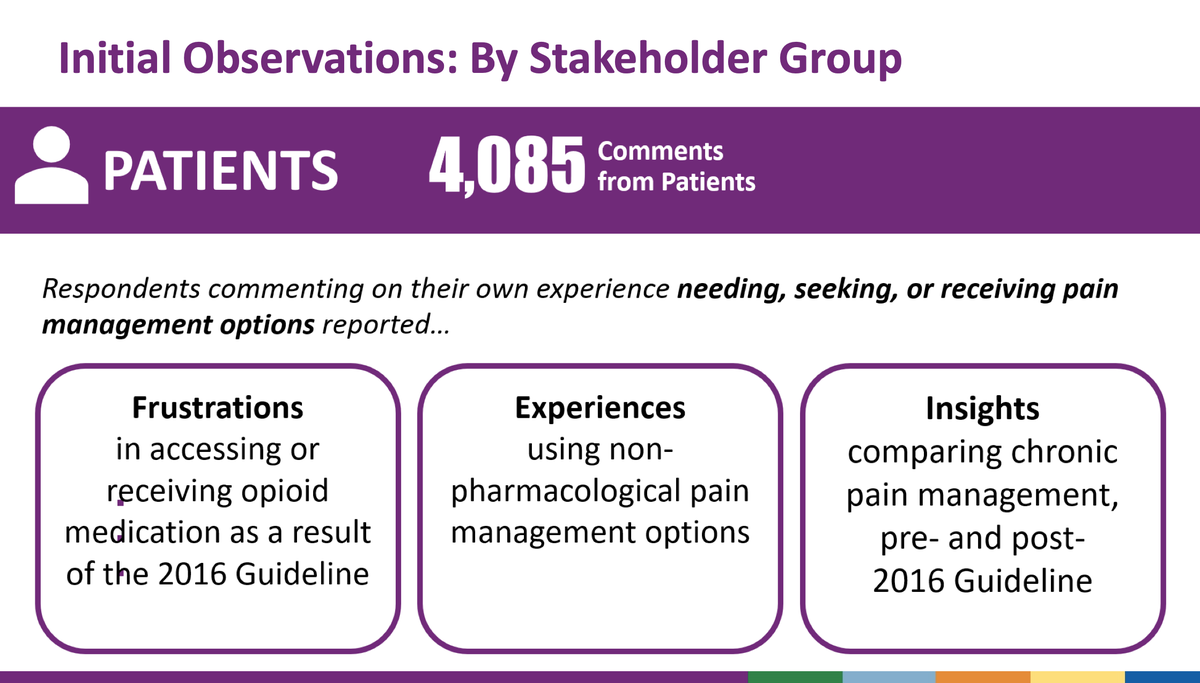
8/Among over 5000 comments received by @CDCgov over 4000 were from patients. Major themes included frustrations receiving pain care, medication, and just general observation
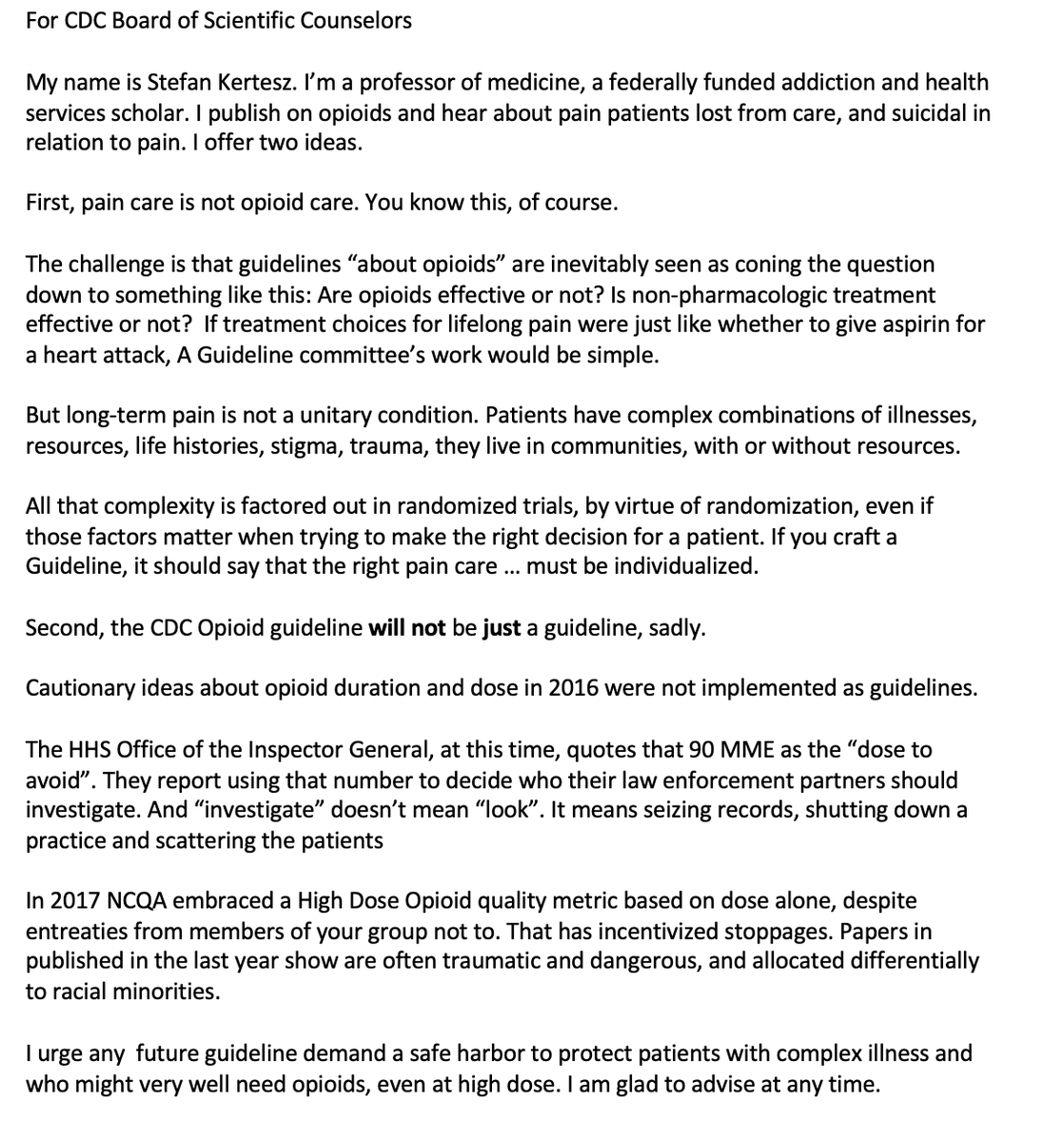
9/Comments to CDC submitted by me, @AjayManhapra @AJ_Gordon are here: https://medium.com/@StefanKertesz/our-response-to-the-cdcs-request-for-comment-on-management-of-acute-and-chronic-pain-5013778f9910
10/Patient @funchefchick underscores that it has been unethical that CDC has no patients (or at most once) on their new opioid Guideline workgroup. And it's unethical to rely on studies of prescription numbers without any clinical context
11/Patient & scholar @NitaGhei highlights that the CDC's emphasis on Rx numbers has left providers unwilling to care for patients with pain. Lack of access to treatment for 20m patients living with high-impact: "we are the biggest stakeholder and we are not represented anywhere"
12/Radiologist David Prologo speaks on behalf of the American College of Radiology to indicate that radiologic procedures reduce pain and can reduce #opioid exposure. Request: add interventional radiologist to work group
13/Patient Fred Brown has been a patient with pain, with 4 surgeries, for over a decade. "Such added stress has been brought about due to the Guidelines. Many of the patients that have been injured are no longer with us". Street Drugs and Suicide.
14/ At this meeting there was no moment of silence fo patients with pain (there was a moment of silence for lives lost due to COVID19 and racism) - details Nuremberg Code of Ethics on involuntary experimentation on patients, says patient @Txsconstitution
15/Patient @PainPtFightBack asks that opioid dose in MME should be evaluated in "terms of the impact on the patient", rather than just judging the dose alone."If you live in my world, I must travel from Alabama to California just to receive medical care"
16/Patient @PainPtFightBack tracks deaths after opioid prescriptions are stopped. Suicide. Heart Attacks. There is NO government agency that tracks, so she does it. "This has become a full time job for me"
17/Patient and 9/11 First Responder and Veteran "Justin" reports that he needed a balanced approach to pain care, and that it's crucial to not allow patients with severe pain to be harmed by excessive opioid prescriptions.
18/Patient and nurse reports that "as a result of the 2016 CDC Guideline, I am not the person I want to be and not the mother I want to be." "All patients should be able to get care without stigma and without being judged"
19/Chris Booth from Mississippi: husband, brother, father, friend, pain patient, who worked in health care. Describes being hit by an 18-wheeler and surgeries that followed.
--off all meds, benefiting from spinal cord stimulation.
--off all meds, benefiting from spinal cord stimulation.
20/Patient @aander1987 "I daily assist abandoned patients who have experienced abrupt discontinuation" - with the 2016 Guideline, "the CDC created a crisis". The reference to specific dose was "weaponized" - "it is harming patients and missing the cause of the overdose crisis"
21/Patient
@aander1987
faults the reliance of CDC reports that report on ONLY
a)insurer
b) dose
c) a single diagnosis code
"Why has the CDC not focused on the impact on individual patients since the Guidelines have been implemented?"
@aander1987
faults the reliance of CDC reports that report on ONLY
a)insurer
b) dose
c) a single diagnosis code
"Why has the CDC not focused on the impact on individual patients since the Guidelines have been implemented?"
22/Next speaker makes the case for "photo biomodulation" as a potential evidence-based therapy for reducing pain. It has some data for post-operative use it seems: https://pubmed.ncbi.nlm.nih.gov/29909435/
23/Dr. Peter Staats led (and leads) pain medicine at Johns Hopkins and served on the @HHSgov pain best practices task force. He puts forward the case for neuromodulation therapy. Urges evidence based approaches.
24/Patient with pain Mary from Washington: had horrific pain experiences starting in 2006. She was given the opportunity to try a spinal cord stimulator in 2013. It was life altering. She wishes she had known about this earlier.
25/Cammie Lavalle is a patient. She had conditions that prohibit technology. She is being force-tapered. She says it's reflective of Minnesota policies.

 Read on Twitter
Read on Twitter