1/ This article ( https://jamanetwork.com/journals/jama/fullarticle/2768396) was recently published in JAMA, and argues against aerosols being an important transmission pathway for COVID-19. Although better than other similar articles, the arguments against aerosols are weak or incorrect. Here we go.
2/ Most important lack of understanding about aerosols. Seems very unlikely it was reviewed by someone with knowledge of aerosol physics or airflow
Most important property of aerosols is size. Bc mass increases with the diam^3, aerosol properties change dramatically w/ size
Most important property of aerosols is size. Bc mass increases with the diam^3, aerosol properties change dramatically w/ size
3/ “Droplets are classically described as larger entities (>5 μm) that rapidly drop to the ground by force of gravity, typically within 3 to 6 feet of the source person.”
But real size for droplets falling that quickly is > 50 μm, so 10 times the size and 1000 (!) times the mass
But real size for droplets falling that quickly is > 50 μm, so 10 times the size and 1000 (!) times the mass
4/ See this video about the real behavior of ~50 μm particles in the air. Not even at that size there is a dramatic fall speed. https://twitter.com/MicroLevitator/status/1283556047471378432
5/ For particles of 5 μm to fall to the air quickly, as in WHO’s video ( https://twitter.com/WHO/status/1244258441880797184), gravity on Earth would have to be 100 times larger than it is. This happens… in the surface of some stars!
6/ If 5 μm particles fell to the ground as in WHO’s video, we wouldn’t have to worry about aerosol (PM) pollution, because a lot of it would fall to the ground so quickly. And we wouldn’t have to worry about Saharan dust reaching Florida, since those particles are often 5-7 μm.
7/ We are also told: “Aerosols are smaller particles (≤5 μm) that [..] are small enough and light enough to remain suspended in the air for hours (analogous to pollen).”
Which is curious, given that pollen ranges in size from 15 to 200 μm! ( https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/pollen#:~:text=Pollen%20is%20the%20male%20gametophyte,is%20generally%20oval%20or%20spherical).
Which is curious, given that pollen ranges in size from 15 to 200 μm! ( https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/pollen#:~:text=Pollen%20is%20the%20male%20gametophyte,is%20generally%20oval%20or%20spherical).
8/ If pollen particles could only follow WHO’s command, we wouldn’t have to worry about allergies either.
Clearly we are as safe with these authors and aerosol mechanics as ppl would be if I just started giving medical advice.
Clearly we are as safe with these authors and aerosol mechanics as ppl would be if I just started giving medical advice.
9/ Next: “6 feet of separation would not provide protection from aerosols that remain suspended in the air or are carried by currents.” This again reveals a lack of understanding about how droplets and aerosols spread and dilute.
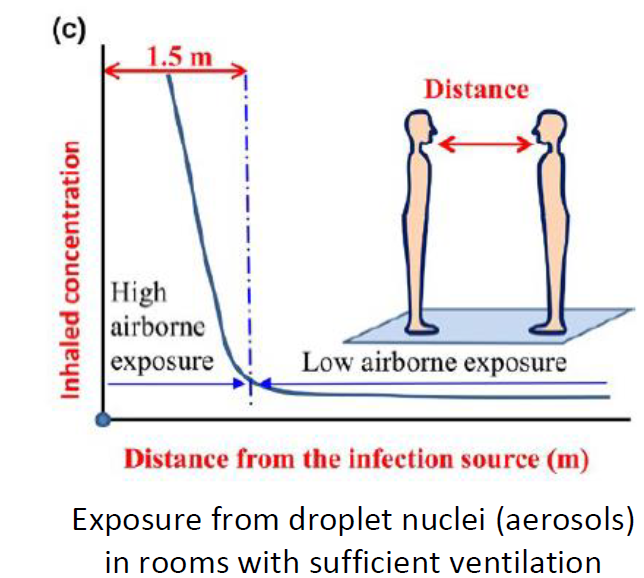
10/ Exhaled aerosols are most concentrated right in front of the nose and mouth, and get diluted strongly with distance by air currents, as illustrated by the schematic below (from https://vbn.aau.dk/ws/portalfiles/portal/332256833/The_influence_of_air_distribution_on_droplet_infection_and_airborne_cross_infection.pdf):
11/ Think about talking with a smoker (smoke is exactly aerosols). If you are at 1 m and the person is just breathing the smoke as in normal breathing, a lot of smoke in between you. Less smoke in the room, but can build up if low ventilation.
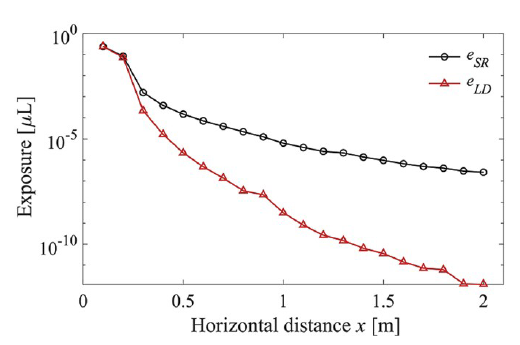
12/ That was a qualitative diagram, but quantitative studies w/ very careful physics ( https://www.sciencedirect.com/science/article/abs/pii/S0360132320302183) estimate exposure to droplets and aerosols vs. distance on close contact situation. The graph below shows the exposure to droplets (black) and aerosols (red) for talking
13/ Aerosols dominate beyond 20 cm, and are larger by x100 at 0.5 m and x2000 at 1 m. A modeling study, but rigorous, using best information on sizes & amounts of expired particles. It has uncertainties… but probably not factors of 100-1000.
14/ Some people argue that importance of close contact as disproving aerosols. But no understanding of details of close contact. Dominant transmission at close contact, rather than disproving aerosols, actually means that they are very likely important or dominant.
15/ Next: “the data [..] are difficult to reconcile with long-range aerosol-based transmission.”
I agree with that, but that is not what we think aerosols are doing for COVID-19. Aerosol transmission, but with much lower contagiousness than e.g. measles (ballpark x 20 less).
I agree with that, but that is not what we think aerosols are doing for COVID-19. Aerosol transmission, but with much lower contagiousness than e.g. measles (ballpark x 20 less).
16/ Lower infectiousness means that aerosols will infect best at close contact when they are most concentrated and one person is inhaling the expired aerosols of the other with limited dilution. Then they have more trouble infecting at the room scale, but they can do so if we...
17/ “help” them accumulate (as smoke), w/ low ventilation, long duration, no masks, talking or singing, as in the Skagit Choir case. We would expect them to really have trouble infecting at very long range, such as through the HVAC system of a building, due to very high dilution
18/ Next: R0 is “quite different from that of viruses that are well known to spread via aerosols such as measles, which has a reproduction number closer to 18.” This argument about R0 is the most repeated argument against aerosols, and it is actually the weakest.
19/ Diseases w/ very high R0 hard to explain except for aerosols. But many people assume that R0 << measles, it means it does not transmit through aerosols! No basis for that assumption. SARS-CoV-2 just much less contagious. To their credit the authors recognize that possibility
20/ Next: low attack rates (rates of new infections, relative to contacts of infected person). Concludes “This pattern seems more consistent with secretions that fall rapidly to the ground within a narrow radius of the infected person rather than with virus-laden aerosols that...
21/ remain suspended in the air at face level for hours where they can be inhaled by anyone in the vicinity.”
This is reflective of the same misunderstanding discussed above. No clear conclusions about the modes of transmission emerge from that observation.
This is reflective of the same misunderstanding discussed above. No clear conclusions about the modes of transmission emerge from that observation.
22/ Virus not very contagious (imagine what the world would look like if transmitted like measles!). Pattern can be explained by the time it takes to breathe enough exhaled aerosols (dose) to lead to infection. Which is much higher at the room scale than the close contact scale
23/ Next: “Proponents of aerosol-based transmission cite well-documented clusters of infections among choir participants, restaurant patrons, and office workers sharing closed indoor spaces. However, based on the reproduction number for SARS-CoV-2, ...
24/ these events appear to be the exception rather than the rule.”
Except that they seem quite common: ( https://www.nytimes.com/2020/06/30/science/how-coronavirus-spreads.html, https://www.nytimes.com/2020/06/02/opinion/coronavirus-superspreaders.html and studies linked therein).
Except that they seem quite common: ( https://www.nytimes.com/2020/06/30/science/how-coronavirus-spreads.html, https://www.nytimes.com/2020/06/02/opinion/coronavirus-superspreaders.html and studies linked therein).
25/ 2 studies quoted: 2% of cases lead to 20% of new transmissions (and 10% -> 80%), R0 = 10-25 for those subsets. High numbers that... are difficult to explain without aerosols! Does not mean it is suddenly like measles, just that right environment: low ventilation, duration etc
26/ Next: possibility of other modes of transmission being at play in reported clusters: “it is difficult to determine in retrospect all the potential person-to-person interactions that may have happened before, during, and immediately following these events.”
27/ Yes, it is difficult. But for the choir case that we investigated ( https://www.medrxiv.org/content/10.1101/2020.06.15.20132027v1), 53 out of 60 were infected in 2.5 h. Most of the time singing in fixed positions, no one within the 2 m landing area of droplets of the index case.
28/ They were aware of COVID-19, no handshakes, sanitizer (and fomites less likely per CDC, WHO: “no specific evidence”). A couple of 10 min breaks. Droplets? Would require extended close contact of 15 min (per CDC) with 53 people!
29/ Explanation other than aerosols requires “contortionist thinking” (B. Nazaroff).
Side point: “Reviewing the literature on large droplet transmission, one can find no direct evidence for large droplets as the route of transmission of any disease” https://www.sciencedirect.com/science/article/pii/S0360132320302183
Side point: “Reviewing the literature on large droplet transmission, one can find no direct evidence for large droplets as the route of transmission of any disease” https://www.sciencedirect.com/science/article/pii/S0360132320302183
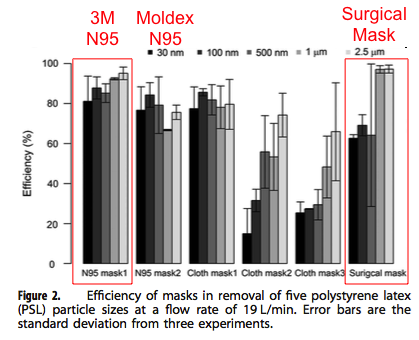
30/ Next: effectiveness of N95 vs surgical masks at reducing transmission in hospital environments. Evidence is unclear about which is better. Authors fail to consider that those masks are not extremely different for > 1 um range most relevant to disease transmission.
31/ One study ( https://www.nature.com/articles/jes201642) found that, a surgical mask performed better than N95 at > 1 um. (Much more different for submicron, i.e. for pollution)
32/ Supermicron particles: trouble making sharp turns. @linseymarr: ~80% well-worn surgical masks. Assume N95 ~ 95% efficient (both at >1um), some imperfect fit. Hospital studies try to measure a small difference in effectiveness w/ lot of confounding factors -->unclear results
33/ Article does recognize some evidence in favor of aerosols. But evidence against aerosols is weak or incorrect. Underlying understanding of aerosols and air flows very limited.
34/ In fact there are many arguments in favor of aerosols, a powerful one being that it is the most consistent with the observed patterns of transmission. See: https://twitter.com/jljcolorado/status/1282970164636483585
35/ See also this thread by Joe Allen on this letter, with more of a building science bent: https://twitter.com/j_g_allen/status/1282998975113699328
36/ Summary: consistent with experience engaging the aerosol skeptics. There are simply no good arguments against aerosol transmission being important for COVID-19. But lack of awareness about aerosol physics, behavior in air, airflows, which leads people to incorrect conclusions
37/ JAMA should engage aerosol reviewers in papers about aerosols. More important, researchers in medicine should collaborate with aerosol res. A lot that we don’t know and that we need to learn. Let’s work together in the future and break down some of these field-field barriers
38/ It seems to me that in medicine "aerosols" = what needs aerosol PPE to stop it. "droplets" = what needs droplet PPE to stop it. But physics much more complex and nuanced, real behavior does not correspond with those names.
39/ Comment if you think my arguments have flaws, explain why, or other info or discussions.
@linseymarr @j_g_allen @CorsIAQ @CathNoakes @ShellyMBoulder @WargockiPawel @SaskiaPopescu @eliowa @RanuDhillon @dan_diekema @jdangjackson
@SamInSilico @raj_mehta @asato4kids
@linseymarr @j_g_allen @CorsIAQ @CathNoakes @ShellyMBoulder @WargockiPawel @SaskiaPopescu @eliowa @RanuDhillon @dan_diekema @jdangjackson
@SamInSilico @raj_mehta @asato4kids
40/ @AbsoluteNorway @jmcrookston @auscandoc
@limhh7 @FraserNeiman @YeahHeyItsSteve @calsandy
@MoNscience @contente_rui @Van_Firth @mlipsitch
@DMuellerID @susaniniowa @mdjkf @TomWalshMD13
@apoorva_nyc @RichReadReports @angie_rasmussen @jksmith34 @jeremyphoward
@limhh7 @FraserNeiman @YeahHeyItsSteve @calsandy
@MoNscience @contente_rui @Van_Firth @mlipsitch
@DMuellerID @susaniniowa @mdjkf @TomWalshMD13
@apoorva_nyc @RichReadReports @angie_rasmussen @jksmith34 @jeremyphoward
41/ @mvankerkhove @allegranzib @WHO @CDCgov
@epireport @CIRESnews @Babak_Javid_Lab
@javisalas @kprather88 @mauricedehond @ErinBromage
@crisperi @WinstonBharatMD @JAMA_current @ProfCharlesHaas @xqcgeo
@epireport @CIRESnews @Babak_Javid_Lab
@javisalas @kprather88 @mauricedehond @ErinBromage
@crisperi @WinstonBharatMD @JAMA_current @ProfCharlesHaas @xqcgeo
42/ Correction: I did mess an important one in tweet 12: aerosols are black, droplets are red. Text is correct.
43/ PS: 1 thing I missed on #25. It could actually be "towards measles" for infrequent ppl that shed a lot more virus. Could also help explain superspreader events, in addition to environment (low ventilation, crowding, duration, no masks, indoors). E.g.: https://www.washingtonpost.com/health/2020/07/18/coronavirus-superspreading-events-drive-pandemic/

 Read on Twitter
Read on Twitter