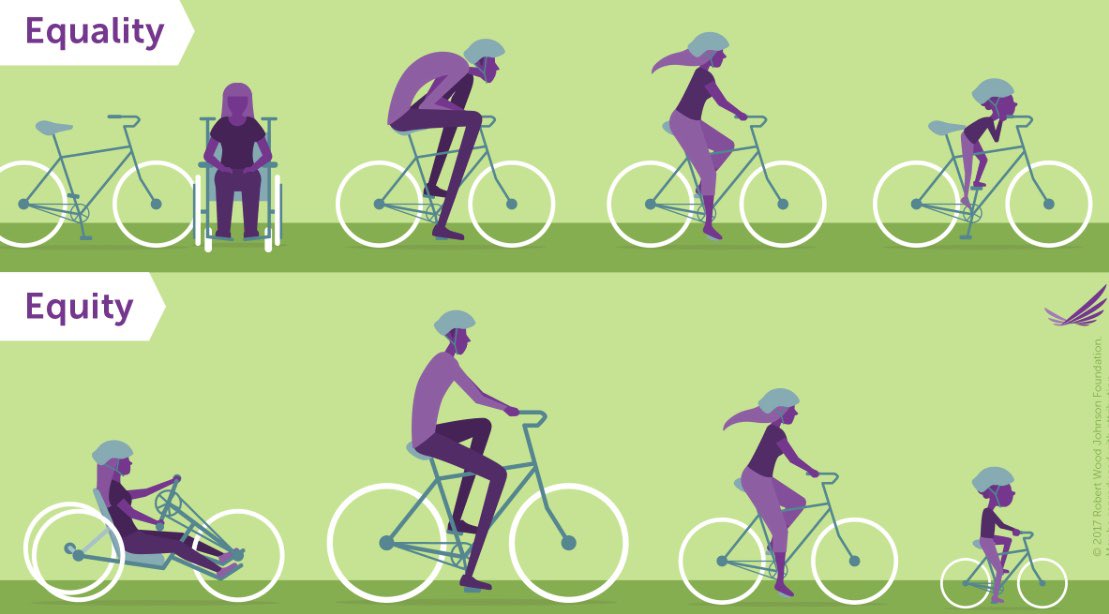
Contact tracing is crucial, but not linear. Failing at any point creates a feedback loop, leading to more cases. And *equity* (not equality) is key. A brief explainer: (1/n)
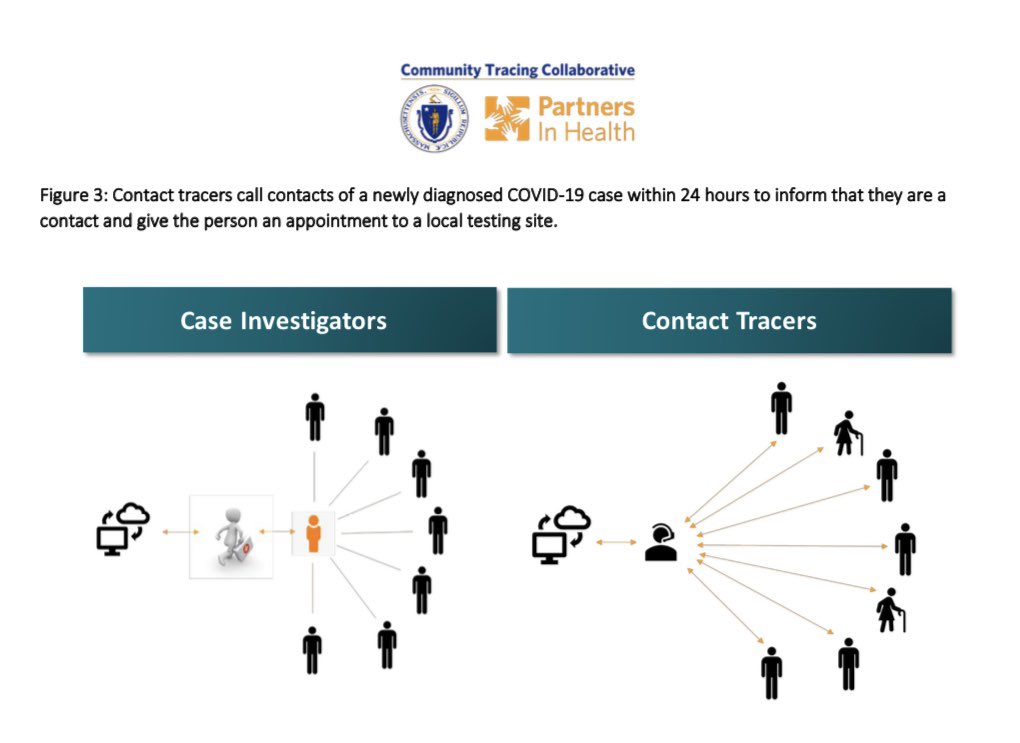
After receiving a positive result, people case/disease investigators help them identify everyone they interacted recently. Then contact tracers reach out to each person identified. (2/n)
But (as expected) not everyone identified/contacted is staying home: (3/n) https://komonews.com/news/coronavirus/only-1-in-5-isolating-when-covid-symptoms-develop-king-county-says
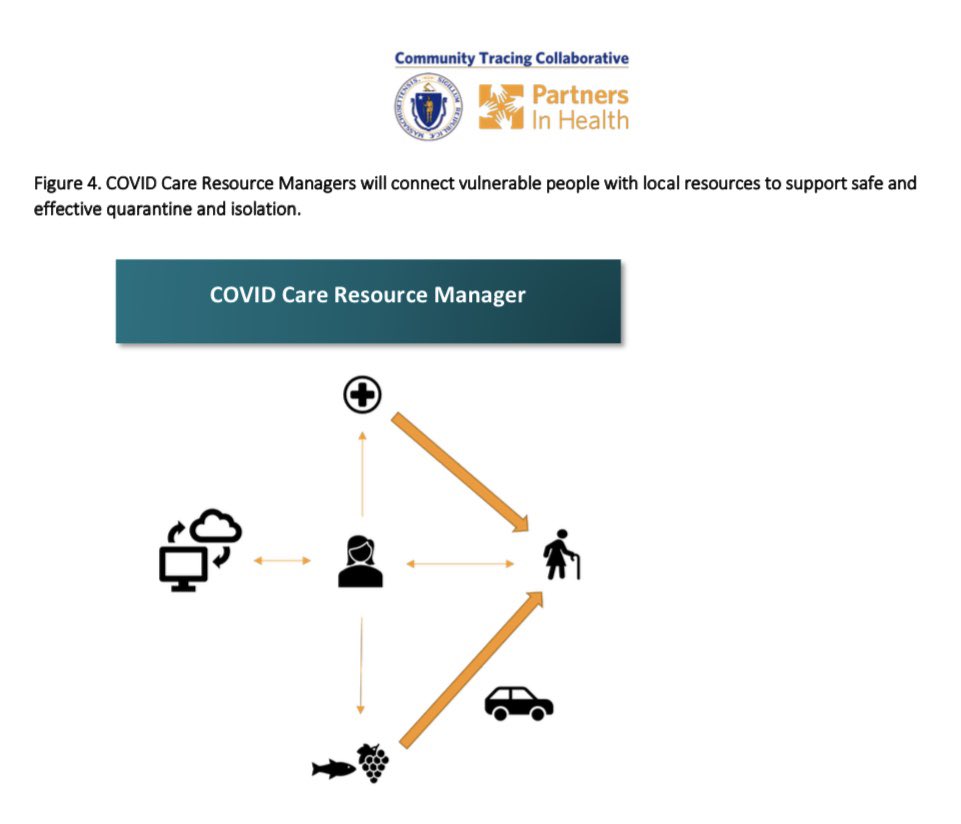
Why? Borrowing from epidemiologists ( @nataliexdean), “think like a sociologist.” What are the *structural impediments* preventing people from self-quarantining? (4/n)
Care resource managers can help fill this need. The @MassDPH and @PIH offers a model for how to do this, depicted below. Everything is available here (5/n) https://www.mass.gov/covid-19-community-tracing-collaborative-resources
@ShreyaKangovi and @uche_blackstock write about the need for *community health workers* in this @washingtonpost OpEd, again addressing concerns about inequities: (6/n) https://twitter.com/shreyakangovi/status/1279401079244013568?s=21 https://twitter.com/shreyakangovi/status/1279401079244013568
And we know that there are policies that we can invest in now to help break the chain of transmission, hazard pay, sick leave, access to hc, liveable wages, etc. (w/ @CourtneyBoen & @RMCarpiano) (7/n) https://thehill.com/blogs/congress-blog/healthcare/494251-inequities-in-covid-19-are-tragic-but-preventable

 Read on Twitter
Read on Twitter