Hi #medtwitter + new onc fellows! I treat patients with advanced #melanoma, especially rare ones like #uvealmelanoma (UM). This #tweetorial will discuss:
1) Why UM is unique
2) When does(n’t) immunotherapy work for UM
3) Why we prefer clinical trials for advanced UM
1/x
1) Why UM is unique
2) When does(n’t) immunotherapy work for UM
3) Why we prefer clinical trials for advanced UM
1/x
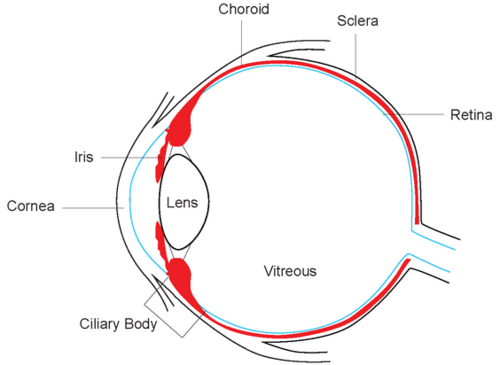
UM affects about 5/million, and about 3-5% of advanced melanomas in the US arise from the uveal tract (iris, ciliary body, choroid). Of these, iris is rarest + least aggressive, so we often call it “choroidal” melanoma.
Get your dilated eye exams, folks!
2/x
Get your dilated eye exams, folks!
2/x
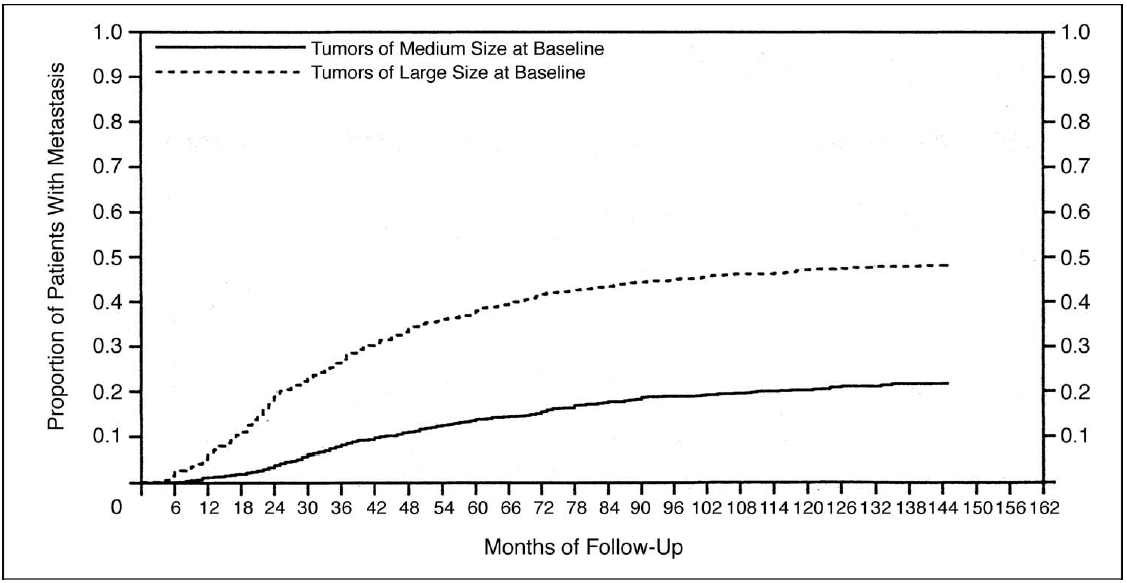
Choroid and cilio-choroid melanomas can be aggressive. ~50% of the largest tumors metastasize; about 20% of medium ones do.
Look at that lack of plateau! Plenty of mets happen late, >5 years out. It's sad but fascinating when immune system controls disease for years, then ( )
)
Look at that lack of plateau! Plenty of mets happen late, >5 years out. It's sad but fascinating when immune system controls disease for years, then (
 )
)
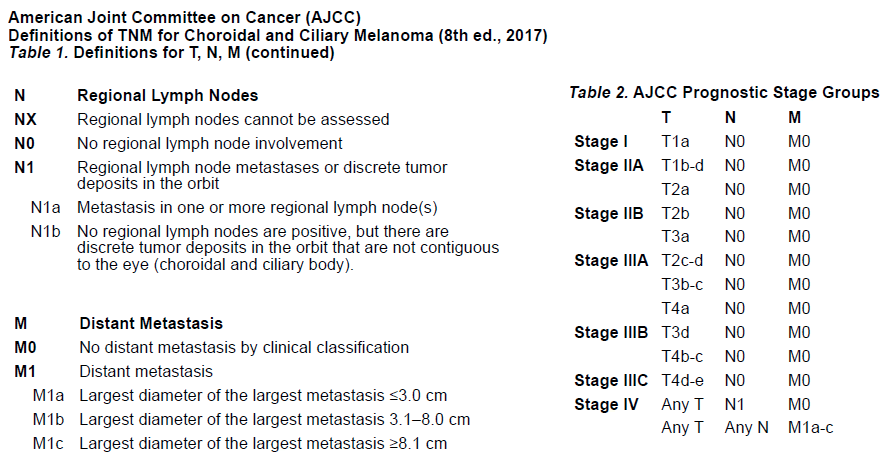
When UM spreads, it most often goes to the liver for reasons we still don’t well understand. Most who die of disease will die of liver failure. For this reason, treatments can be PO/IV or just liver-directed. UM AJCC staging reflects size, not site of met (unlike skin mel).
4/x
4/x
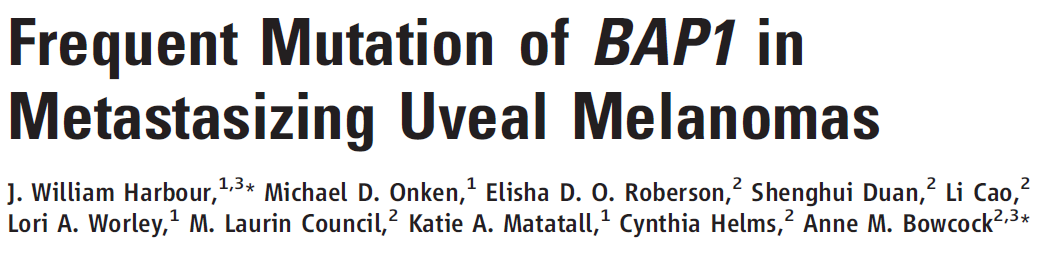
Primary UM biology is fascinating. Labs like Bastian and @JWHarbourMD have molecularly defined primary UM since mid-2000s. The highest risk primary tumors can be molecularly defined: BAP1 > SF3B1 >> EIF1AX, 3p loss, RNA profiling. No BRAF V600 mutants.
5/x
5/x
Genomic risk stratification changed surveillance patterns starting in late 2000s. Most pts were getting no surveillance; now, CT/MRIs of liver are common, esp if known high risk. This has important implications for interpreting survival data later.
https://bjo.bmj.com/content/97/2/159.long
6/x
https://bjo.bmj.com/content/97/2/159.long
6/x
So if they metastasize, what then? If you read no further, remember: send them to me or another referral center. I won’t discuss the revolution in cutaneous melanoma driven by #Immunotherapy or BRAF V600-targeted therapy; I assume you’ve seen @NobelPrize announcements. 7/x
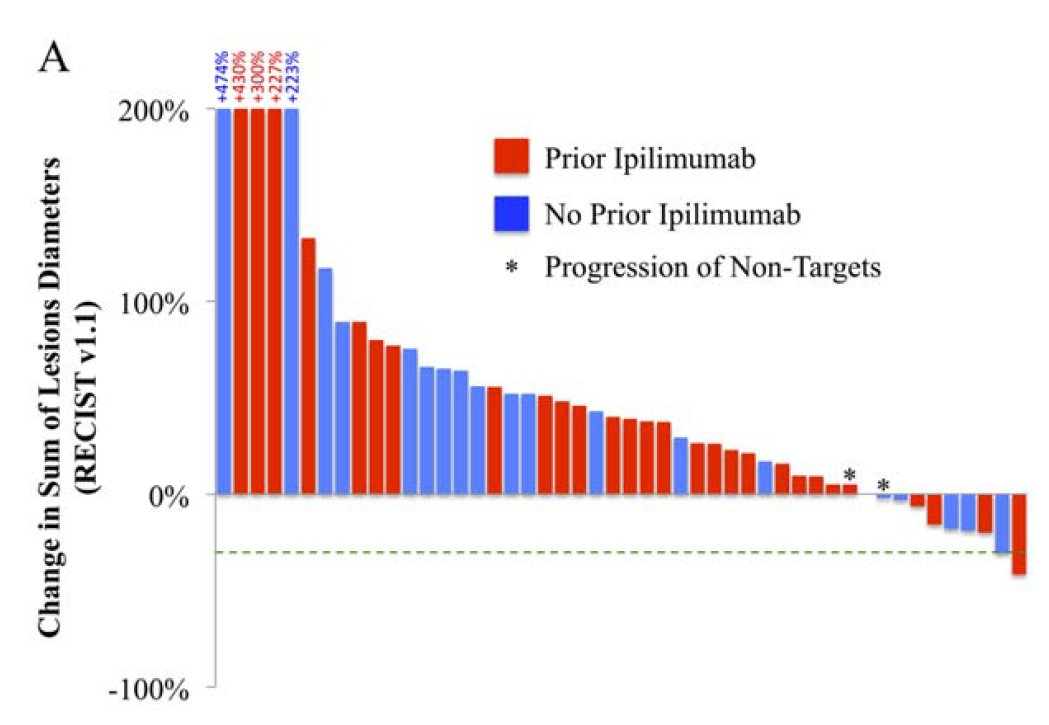
This revolution has largely left behind our patients with #uvealmelanoma. Why? Early data with CTLA-4 inhibitor ipilimumab looked to help ~5% shrink tumors…similar to skin melanomas. So many of us felt rapid improvements were just around the corner. 8/x https://acsjournals.onlinelibrary.wiley.com/doi/full/10.1002/cncr.28282
But PD-1 blockade, a blockbuster in skin melanomas and many other tumors, was a decided dud. Only 4% response in (mainly) 2nd/3rd line retrospective study! Median OS from 2nd/3rd line was dismal, 8mo. 9/x
https://acsjournals.onlinelibrary.wiley.com/doi/full/10.1002/cncr.30258
https://acsjournals.onlinelibrary.wiley.com/doi/full/10.1002/cncr.30258
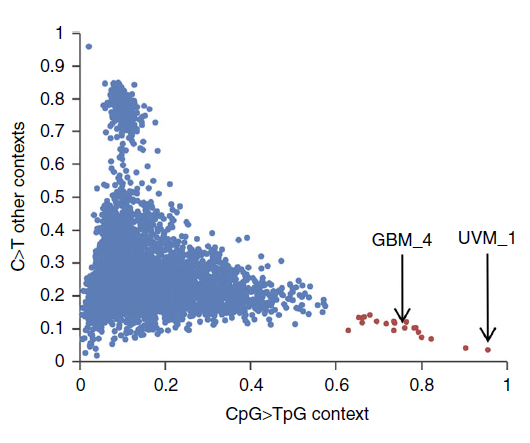
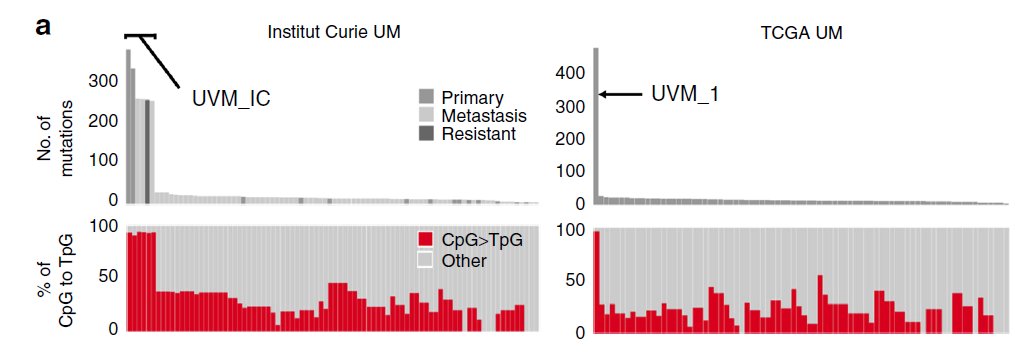
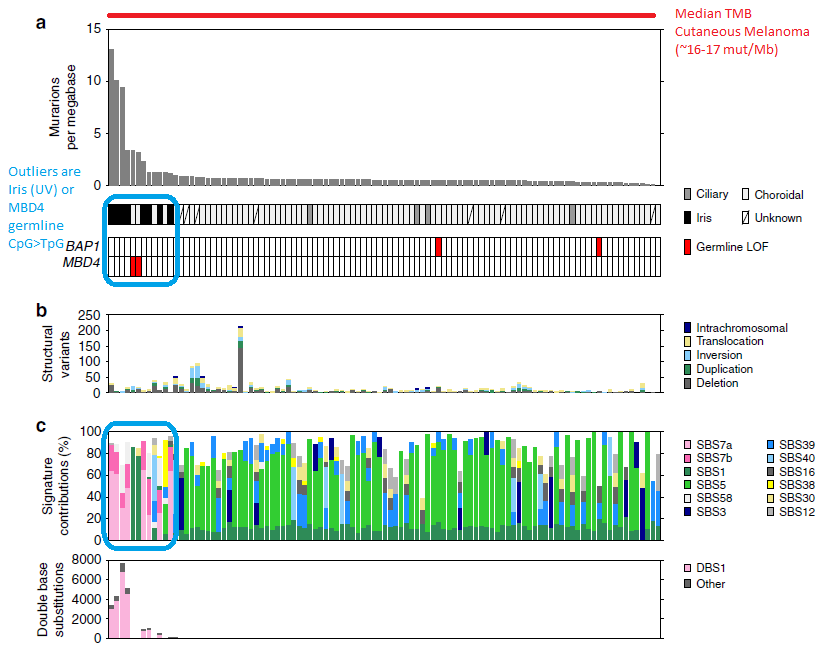
PD-1 blockade occasionally had durable responses, but molecular analysis recently showed genomic outliers in 2 cases with hypermutation and novel germline mutation in MBD4. Cool biology, seen in other neoplasms too, but not useful for most patients.
https://www.nature.com/articles/s41467-018-04322-5
10/x
https://www.nature.com/articles/s41467-018-04322-5
10/x
I picked most recent whole genome study from our Aussie friends that confirms many prior studies: primary UMs have a low, low, low tumor mutation burden (TMB). Outliers were only in iris (sun-exposed) or rare MBD4 germline carriers.
11/x
https://www.nature.com/articles/s41467-020-16276-8
11/x
https://www.nature.com/articles/s41467-020-16276-8
OK so the "high TMB/T cell inflamed=PD-1 mono-tx" paradigm won't work. But what about combined PD-1 + CTLA-4 blockade with nivolumab + ipilimumab (nivo+ipi)? It has a track record of response in a subset of tumors where PD-1 doesn’t work alone. (fCOI: I consult for BMS)
12/x
12/x
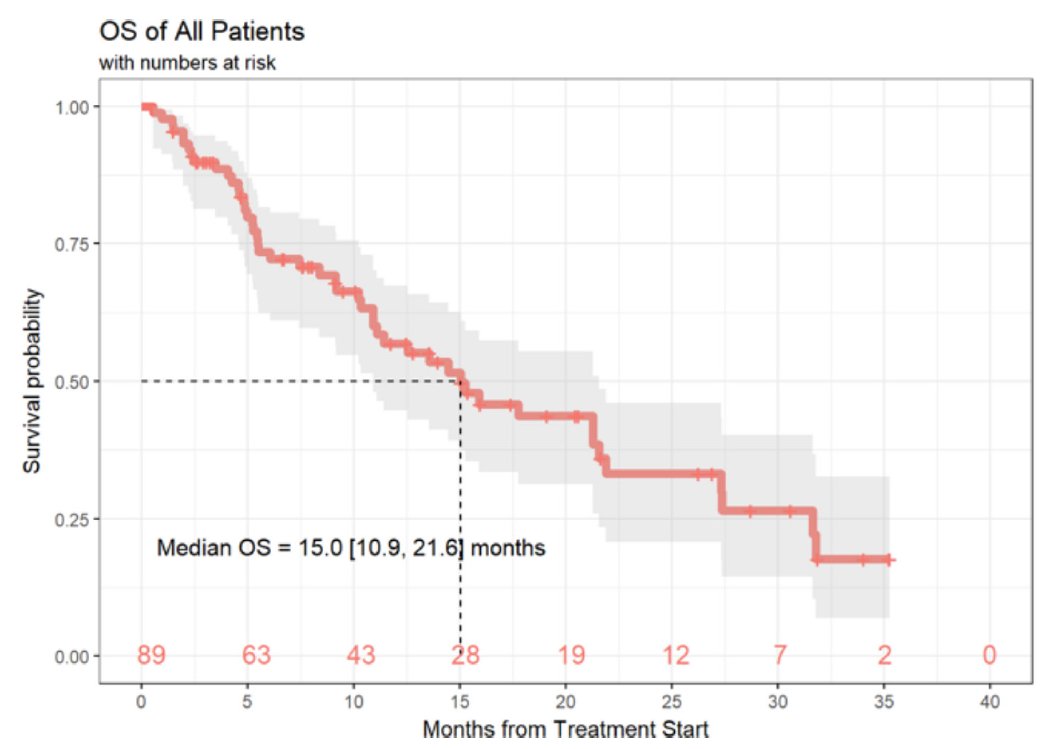
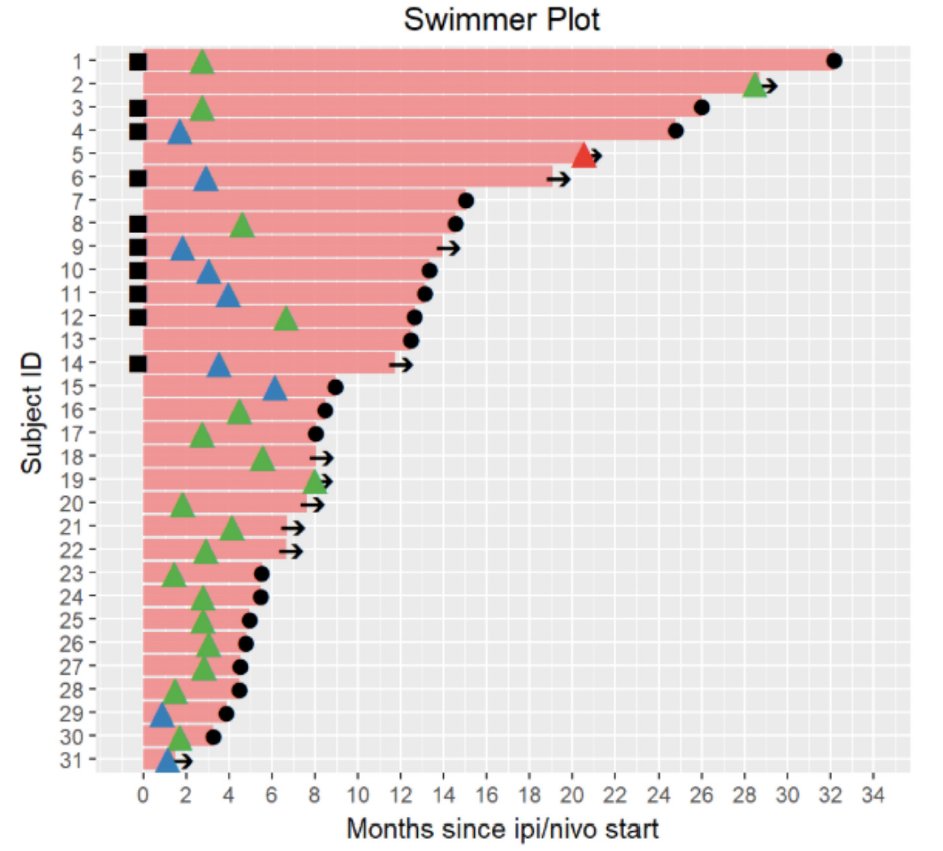
There are now 2 retrospective reports of nivo+ipi in UM; one US-based ( @YanaNajjarMD @FunchainMD, others) and one Europe-based . ORR in both is low, 12-16% (vs skin ORR 55-60%). Toxicity looked just as high, unfortunately.
https://jitc.biomedcentral.com/articles/10.1186/s40425-019-0800-0
https://jitc.bmj.com/content/8/1/e000331.long
13/x
https://jitc.biomedcentral.com/articles/10.1186/s40425-019-0800-0
https://jitc.bmj.com/content/8/1/e000331.long
13/x
When patient tumors shrink, they can stay shrunk for a while: median duration was 25 months in European cohort. In our cohort, it was only 6 months (but small numbers, short f/u). So nivo+ipi can be a good option for a small subset of pts. We just don't know which ones. 14/x
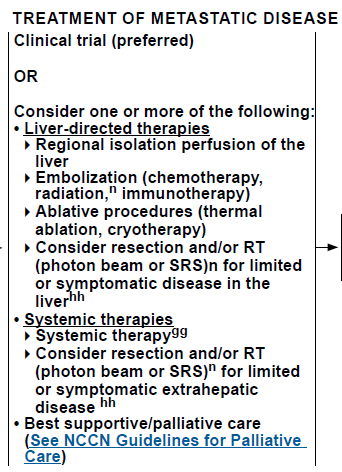
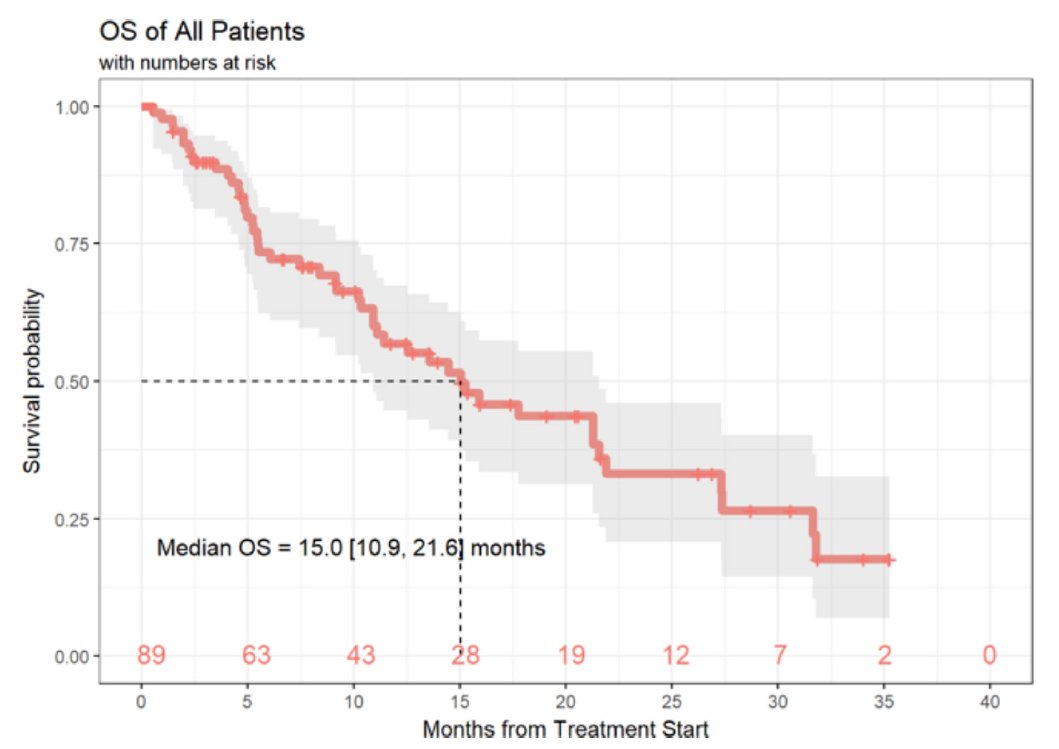
So, with this median OS climbing from historical 6-12 mo to now 15 mo, have we shifted the standard of care? Is nivo + ipi the best option for patient with new UM? The answer is, unequivocally, NO. Clinical trials remain the standard. @NCCN guidelines agree:
15/x
15/x
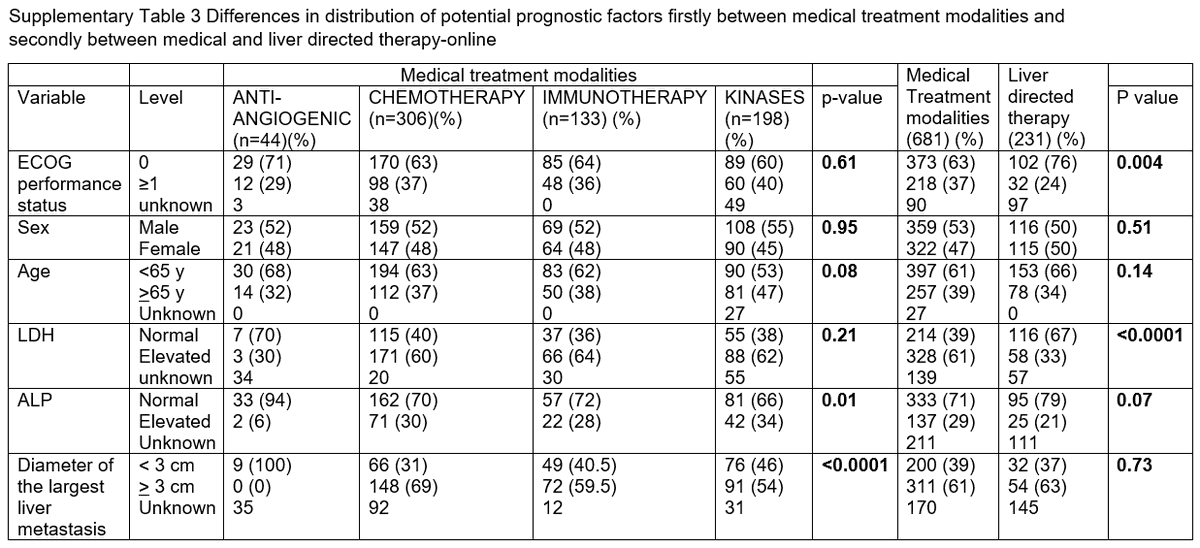
If we are improving OS w/ nivo+ipi, we need to understand historical comparisons. Best data come from meta-analysis of 912 pts known by us cool kids as PUMMA.
Size of metastases (>3cm vs <3cm), blood values (LDH, alk phos), ECOG PS are prognostic.
16/x https://www.sciencedirect.com/science/article/pii/S0923753419312906
Size of metastases (>3cm vs <3cm), blood values (LDH, alk phos), ECOG PS are prognostic.
16/x https://www.sciencedirect.com/science/article/pii/S0923753419312906
Overall OS ~10.2 months. Systemic tx, 9-11 months. Liver-directed therapy -> better OS, but population is also much less sick than those in systemic tx. So can’t say one is better…but we can power current prospective single-arm trials against this benchmark. 17/x
BUT, onc fellows, friends: pitfalls abound. Lots of missing data = ?confounders. Also, trials span from 2003 – 2018.
I suspect that we are catching tumors a lot earlier in 2020 than we were in 2003. Molecular risk stratification, MRIs/CTs improved.
Lead time bias? 18/x
I suspect that we are catching tumors a lot earlier in 2020 than we were in 2003. Molecular risk stratification, MRIs/CTs improved.
Lead time bias? 18/x
If nivo+ipi were improving OS despite lead-time bias, I would need to see a durable tail, like the one we see in Checkmate-067. Do we see one in advanced UM? The answer, unfortunately, is no.
So we must keep searching for novel options. 19/x
So we must keep searching for novel options. 19/x
We improve care by finding signals in Phase 1 trials. Tebentafusp is a nice example (fCOI: personal fees from @Immunocore). UM responded in Ph1  Ph1 expansion
Ph1 expansion  registrational *randomized* Ph2 against MD choice of pembro/ipi/chemo.
registrational *randomized* Ph2 against MD choice of pembro/ipi/chemo.
OS primary endpt. Progress!
20/x
 Ph1 expansion
Ph1 expansion  registrational *randomized* Ph2 against MD choice of pembro/ipi/chemo.
registrational *randomized* Ph2 against MD choice of pembro/ipi/chemo.OS primary endpt. Progress!
20/x
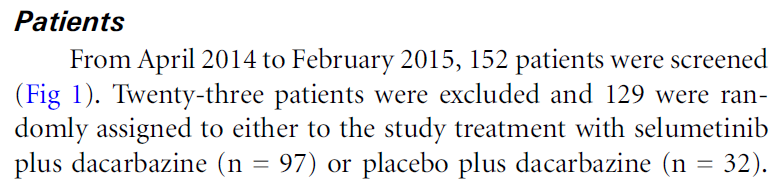
The #uvealmelanoma community is REALLY good at filling large randomized trials internationally w/ @MRFCureOM, the International Rare Cancer Initiative, @MelanomaReAlli . The last large trial (negative...  ), chemo + MEK vs chemo, accrued in ten months!!! We can do it! 21/x
), chemo + MEK vs chemo, accrued in ten months!!! We can do it! 21/x
 ), chemo + MEK vs chemo, accrued in ten months!!! We can do it! 21/x
), chemo + MEK vs chemo, accrued in ten months!!! We can do it! 21/x
But many companies have decided that UM is not worth investigating, even in a Phase 1 “safety” study. Today I counted 68 current Ph1 melanoma studies on http://clinicaltrials.gov (excluding BRAF V600). 26 (38%) explicitly excluded uveal.
22/x
22/x
To all my pharma friends: this is a BIG mistake. No big differences in safety risks for UM vs skin melanoma, so Phase 1 studies should enroll these pts. Who knows, you might get lucky and find a signal for a true orphan indication! Win-win!
23/x
23/x
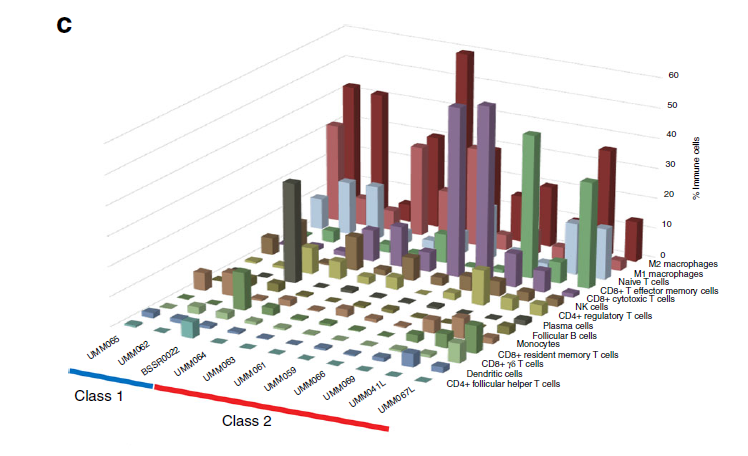
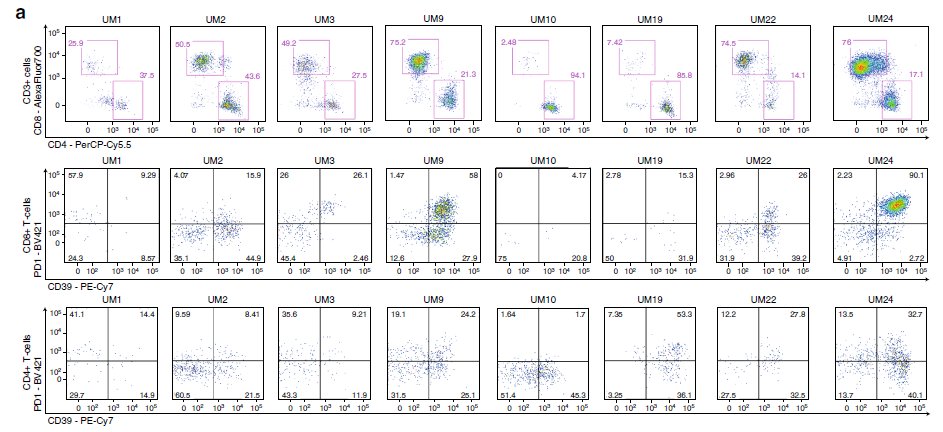
Dear immunotherapy Ph1 designers, the field has debunked the notion that UM is an immunologic “desert.” Beautiful recent work by both @JNilsson_lab and @JWHarbourMD has shown plenty of infiltrates in UM mets. Let us in!
https://www.nature.com/articles/s41467-020-15606-0
https://www.nature.com/articles/s41467-019-14256-1
24/x
https://www.nature.com/articles/s41467-020-15606-0
https://www.nature.com/articles/s41467-019-14256-1
24/x
We know that adoptive TIL at @theNCI (now at @UPMC) has had preliminary success as well: https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(17)30251-6/fulltext
25/x
25/x

 Read on Twitter
Read on Twitter