Antibody tests for identification of current and past infection with SARS‐CoV‐2 - Deeks, JJ - 2020 | Cochrane Library https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD013652/full#.XvTDGHEkVz4.twitter
Living Cochrane Review of Antibody Tests – 1st version now published. Twitter summary to save you reading the 300+ pages
Living Cochrane Review of Antibody Tests – 1st version now published. Twitter summary to save you reading the 300+ pages
#1 Search date of 27 April 2020. Scanned 10,965 COVID-19 publications and pre-prints. Included 54 studies of test accuracy of COVID-19 antibody tests. Some studies looked at multiple tests, so total of 89 test evaluations including 15,976 samples (8,256 from COVID-19 patients)
#2 Most research studies done in China on tests developed and manufactured in China. Data found for 27 commercial tests and 25 in-house assays. 61% were lab assays (requiring venous blood), 39% with point-of-care assays (possible finger-prick blood)
#3 81% of studies done in hospitalised populations – likely to have had the highest antibody responses. Results may not apply to general public who have had milder disease
#4 Most studies (61%) restricted to confirmed COVID-19 cases. Probable COVID-19 cases (as defined by WHO and CDC China) were excluded. Thus samples biased to the clearest cases.
#5 48 (89%) studies identified COVID-19 cases separately from non-cases. Only 6 studies used a “single-gate” type designing, recruiting patients as a cohort before identifying COVID-19 status. More studies like this needed please.
#6 So quality of evidence looks poor. Lots of red and yellow on the QUADAS plot, so please treat any numbers which follow with caution. Lots more to read in the review about this
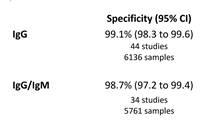
#7 High heterogeneity in sensitivity for IgG, IgM and IgG/IgM (range 0-100%) driven by differences in time since onset of symptoms. Tests really poor in week 1 (30% sens), a bit better in week 2 (65%) before hitting best performance (80-90%) in week 3
#8 we’ve abandoned studies which did not allow stratification of sensitivity by week since onset of symptoms. That’s thrown out lots of studies, many of which may have misleadingly concluded tests were poor because they included people from early weeks without stratification.
#9 also little data beyond 35 days. Don’t know how these tests will hold up for longer duration seroprevalence surveys, or testing for infection which might have occured >5 weeks ago. Antibodies will wain and we don't know when.
#11 Other problems included (a) unstated numbers of multiple samples taken from patients in many studies; (b) very rare for tests to be evaluated using blinding; (c) no mentions of exclusions; (d) use of laboratories and venous blood to evaluate finger-prick POC tests.
#12 Also clear evidence of publication bias as reported previously (from National COVID-19 testing panel)
#13 And nobody seems to have heard of STARD – not a single patient flow-diagram in the 54 studies. Reporting quality was shockingly poor.
#14 Bottom lines:
(A)TIMING REALLY MATTERS. Don’t use the test before 2 weeks. Studies which have done so many wrongly have decided some tests are useless.
(A)TIMING REALLY MATTERS. Don’t use the test before 2 weeks. Studies which have done so many wrongly have decided some tests are useless.
#15 (B)TEST COULD HELP IDENTIFY COVID-19 IN PATIENTS WITH SYMPTOMS FOR >2 WEEKS. This could be useful given the lack of PCR testing in patients who suffered at home without a test, some of whom may still be sick and need medical care. Is anybody doing this?
#16 (C)WE DON’T KNOW WHETHER IT KEEPS WORKING > 5 WEEKS hopefully we’ll find some longer follow-up studies soon.
#17 (D)WE DON’T KNOW HOW WELL THEY WORK IN PATIENTS WITH MILD SYMPTOMS WHO WEREN’T HOSPITALISED hopefully we’ll find some studies in these groups soon
#18 (E)FIGURES FOR SENS AND SPEC MAY BE OVERESTIMATES BECAUSE OF MANY FLAWS IN STUDIES we need to move on and do studies in clinical pathways in representative groups
#19 (F)WE NEED TO UPDATE THE REVIEW WITH DATA FROM MAY AND JUNE ASAP its underway, we now know what we’re doing so hopefully we can be quick!
#20 and thanks to the many colleagues @TERG and in Cochrane groups in the Netherlands, Belgium and Switzerland, and Cochrane Editorial Team who helped do this – it was rapid because we've worked hard - not because of short cuts. We’re going to have a zoom drink to celebrate now!
@threadreaderapp unroll

 Read on Twitter
Read on Twitter