Do you often check a FeNa when working up a patient with AKI?
In my experience it’s ordered reflexively
But is this a good idea? Is a FeNa actually useful?
Let’s find out #NSMCInternship #nephtwitter #tweetorial
Poll!
To differentiate between prerenal AKI and ATN you would
In my experience it’s ordered reflexively
But is this a good idea? Is a FeNa actually useful?
Let’s find out #NSMCInternship #nephtwitter #tweetorial
Poll!
To differentiate between prerenal AKI and ATN you would
In normal circumstances sodium excretion = dietary intake
 What goes in must come out = extracellular volume is maintained within a narrow range
What goes in must come out = extracellular volume is maintained within a narrow range
 Volume →
Volume →  RAAS →
RAAS → sodium excretion
sodium excretion
 Volume →
Volume →  ANP →
ANP →  sodium excretion
sodium excretion
 So why not just use UNa as a surrogate?
So why not just use UNa as a surrogate?
 What goes in must come out = extracellular volume is maintained within a narrow range
What goes in must come out = extracellular volume is maintained within a narrow range Volume →
Volume →  RAAS →
RAAS → sodium excretion
sodium excretion Volume →
Volume →  ANP →
ANP →  sodium excretion
sodium excretion So why not just use UNa as a surrogate?
So why not just use UNa as a surrogate?
 Remember UrNa is affected by concentration (hint: units are mEq/L)
Remember UrNa is affected by concentration (hint: units are mEq/L)Dilute urine =
 UNa even if excretion is high
UNa even if excretion is highConcentrated urine =
 UNa even if total excretion is low
UNa even if total excretion is low FeNa provides a measure of sodium handling that is INDEPENDENT of urinary concentration
FeNa provides a measure of sodium handling that is INDEPENDENT of urinary concentration
FeNa Fact: First described in 1976 by Espinel
17 patients with oliguric AKI
Established current criteria:
<1% for pre-renal
>3% for acute tubular injury (in between values are considered indeterminate)
 Read the original article https://jamanetwork.com/journals/jama/article-abstract/347299
Read the original article https://jamanetwork.com/journals/jama/article-abstract/347299
17 patients with oliguric AKI
Established current criteria:
<1% for pre-renal
>3% for acute tubular injury (in between values are considered indeterminate)
 Read the original article https://jamanetwork.com/journals/jama/article-abstract/347299
Read the original article https://jamanetwork.com/journals/jama/article-abstract/347299
Premise:

 Volume→neurohumoral activation→
Volume→neurohumoral activation→ sodium reabsorption=
sodium reabsorption= excretion
excretion
 Tubular injury→
Tubular injury→ number of functional nephrons to excrete sodium load=
number of functional nephrons to excrete sodium load= FeNa
FeNa
 If GFR didn't
If GFR didn't  with impaired tubular absorption= kidney catastrophe (hence oliguria)
with impaired tubular absorption= kidney catastrophe (hence oliguria)
 https://www.amjmed.com/article/0002-9343(76)90365-X/pdf
https://www.amjmed.com/article/0002-9343(76)90365-X/pdf

 Volume→neurohumoral activation→
Volume→neurohumoral activation→ sodium reabsorption=
sodium reabsorption= excretion
excretion Tubular injury→
Tubular injury→ number of functional nephrons to excrete sodium load=
number of functional nephrons to excrete sodium load= FeNa
FeNa If GFR didn't
If GFR didn't  with impaired tubular absorption= kidney catastrophe (hence oliguria)
with impaired tubular absorption= kidney catastrophe (hence oliguria) https://www.amjmed.com/article/0002-9343(76)90365-X/pdf
https://www.amjmed.com/article/0002-9343(76)90365-X/pdf
Let’s about these numbers. What’s my FeNa right now?
about these numbers. What’s my FeNa right now?
Assume I have a normal GFR of 125 mL/min SNa of 140 mEq/L
SNa of 140 mEq/L
I’m filtering 180L/d x 140 mEq/L=25k mEq/d of sodium
If I ingest 4g of sodium=172 mEq MY FeNa is 0.68%
But I feel fine, and don’t need a bolus, I don’t think..
 about these numbers. What’s my FeNa right now?
about these numbers. What’s my FeNa right now?Assume I have a normal GFR of 125 mL/min
 SNa of 140 mEq/L
SNa of 140 mEq/LI’m filtering 180L/d x 140 mEq/L=25k mEq/d of sodium
If I ingest 4g of sodium=172 mEq MY FeNa is 0.68%
But I feel fine, and don’t need a bolus, I don’t think..

For my FeNa to be >3% (assuming my dietary intake stays constant) I would need to reduce my GFR to at most 28 mL/min.
Therefore the APPLICATION of this formula is contingent on a patient having significant AKI
Therefore the APPLICATION of this formula is contingent on a patient having significant AKI
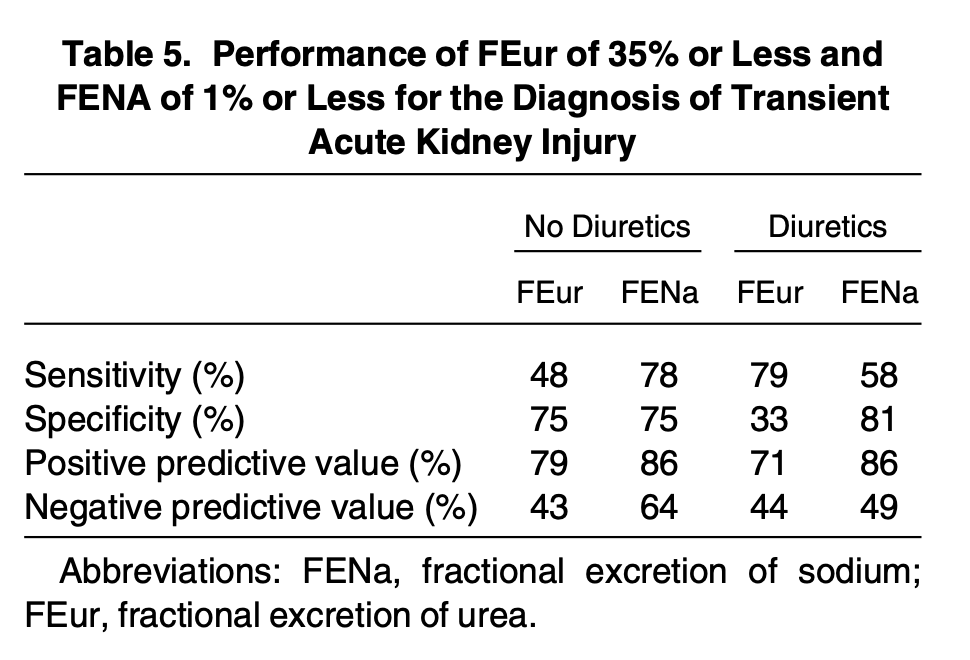
Subsequent studies have shown variable levels of performance as shown with its sensitivity and specificity in the below table 
 It tends to consistently test well in prerenal patients who are oliguric
It tends to consistently test well in prerenal patients who are oliguric

 It tends to consistently test well in prerenal patients who are oliguric
It tends to consistently test well in prerenal patients who are oliguric
Patient on diuretics? No problem get a FeUrea right?
Same principle as FeNa but urea primarily reabsorbed in the proximal tubule=unaffected by traditional (loop and thiazide) diuretics
Volume depletion= urea reabsorption=classic 20:1 BUN to creatinine ratio in a prerenal state
urea reabsorption=classic 20:1 BUN to creatinine ratio in a prerenal state
Same principle as FeNa but urea primarily reabsorbed in the proximal tubule=unaffected by traditional (loop and thiazide) diuretics
Volume depletion=
 urea reabsorption=classic 20:1 BUN to creatinine ratio in a prerenal state
urea reabsorption=classic 20:1 BUN to creatinine ratio in a prerenal state
FeUrea Fact:  described by Kaplan and Kohn in 1992
described by Kaplan and Kohn in 1992
 Retrospective review
Retrospective review
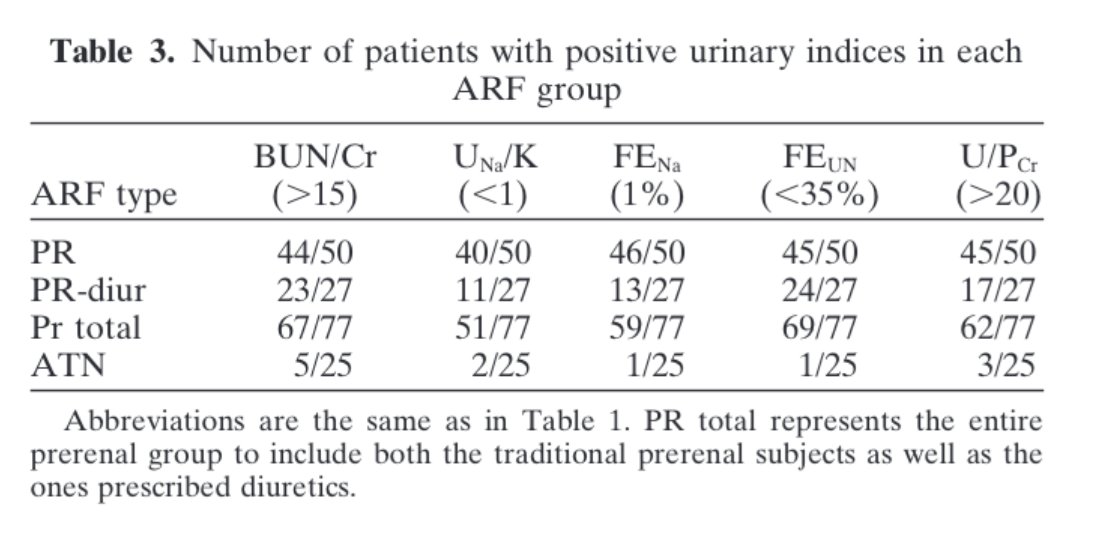
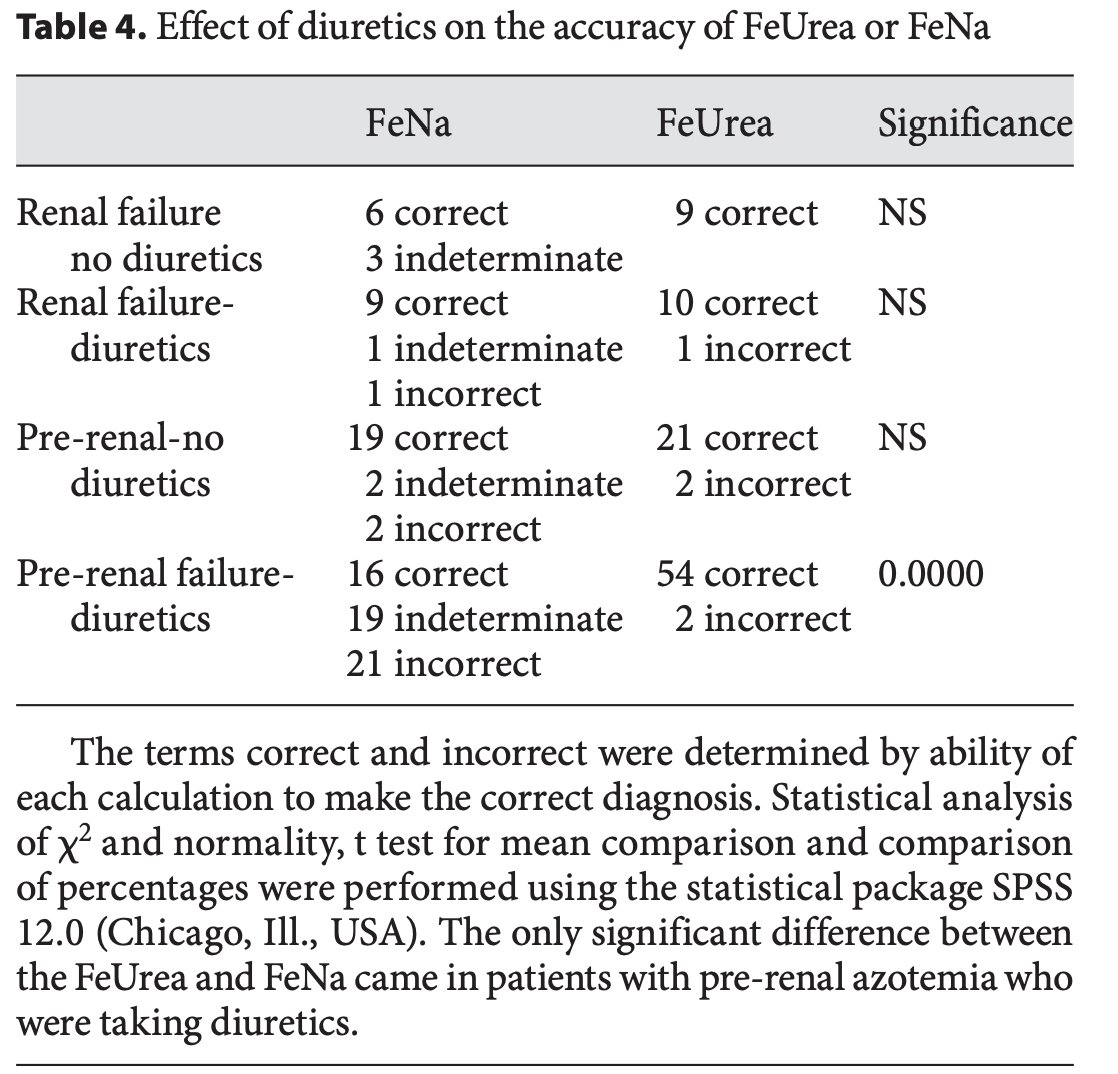
-87 patients,40 with discordant FeNa and FeUrea results,39 treated with diuretics
 Similar efficacy in prerenal pts w/o diuretics but FeUrea>>FeNa in prerenal pts w/diuretics
Similar efficacy in prerenal pts w/o diuretics but FeUrea>>FeNa in prerenal pts w/diuretics
 …https://www-karger-com.offcampus.lib.washington.edu/Article/Abstract/168417
…https://www-karger-com.offcampus.lib.washington.edu/Article/Abstract/168417
 described by Kaplan and Kohn in 1992
described by Kaplan and Kohn in 1992 Retrospective review
Retrospective review-87 patients,40 with discordant FeNa and FeUrea results,39 treated with diuretics
 Similar efficacy in prerenal pts w/o diuretics but FeUrea>>FeNa in prerenal pts w/diuretics
Similar efficacy in prerenal pts w/o diuretics but FeUrea>>FeNa in prerenal pts w/diuretics …https://www-karger-com.offcampus.lib.washington.edu/Article/Abstract/168417
…https://www-karger-com.offcampus.lib.washington.edu/Article/Abstract/168417
Is FeUrea effective?
 Consistently beats FeNa in pts on diuretics, with variable overall efficacy
Consistently beats FeNa in pts on diuretics, with variable overall efficacy
 See tables
See tables 
 Exception: FeNa outperformed FeUrea in septic patients
Exception: FeNa outperformed FeUrea in septic patients
Why? Cytokine stimulation decreases urea excretion by urea transporters
urea transporters
 https://journals.physiology.org/doi/pdf/10.1152/ajprenal.00460.2006
https://journals.physiology.org/doi/pdf/10.1152/ajprenal.00460.2006
 Consistently beats FeNa in pts on diuretics, with variable overall efficacy
Consistently beats FeNa in pts on diuretics, with variable overall efficacy See tables
See tables 
 Exception: FeNa outperformed FeUrea in septic patients
Exception: FeNa outperformed FeUrea in septic patientsWhy? Cytokine stimulation decreases urea excretion by
 urea transporters
urea transporters https://journals.physiology.org/doi/pdf/10.1152/ajprenal.00460.2006
https://journals.physiology.org/doi/pdf/10.1152/ajprenal.00460.2006
So why such variability in performance with both tests?
 The key is patient selection
The key is patient selection
 There are a large number of factors that limit utility for both tests, many of which are common conditions in hospitalized patients, as shown
There are a large number of factors that limit utility for both tests, many of which are common conditions in hospitalized patients, as shown 
 The key is patient selection
The key is patient selection There are a large number of factors that limit utility for both tests, many of which are common conditions in hospitalized patients, as shown
There are a large number of factors that limit utility for both tests, many of which are common conditions in hospitalized patients, as shown 
So is there a better way?
This paper:
 …https://cjasn-asnjournals-org.offcampus.lib.washington.edu/content/clinjasn/3/6/1615.full.pdf?with-ds=yes
…https://cjasn-asnjournals-org.offcampus.lib.washington.edu/content/clinjasn/3/6/1615.full.pdf?with-ds=yes
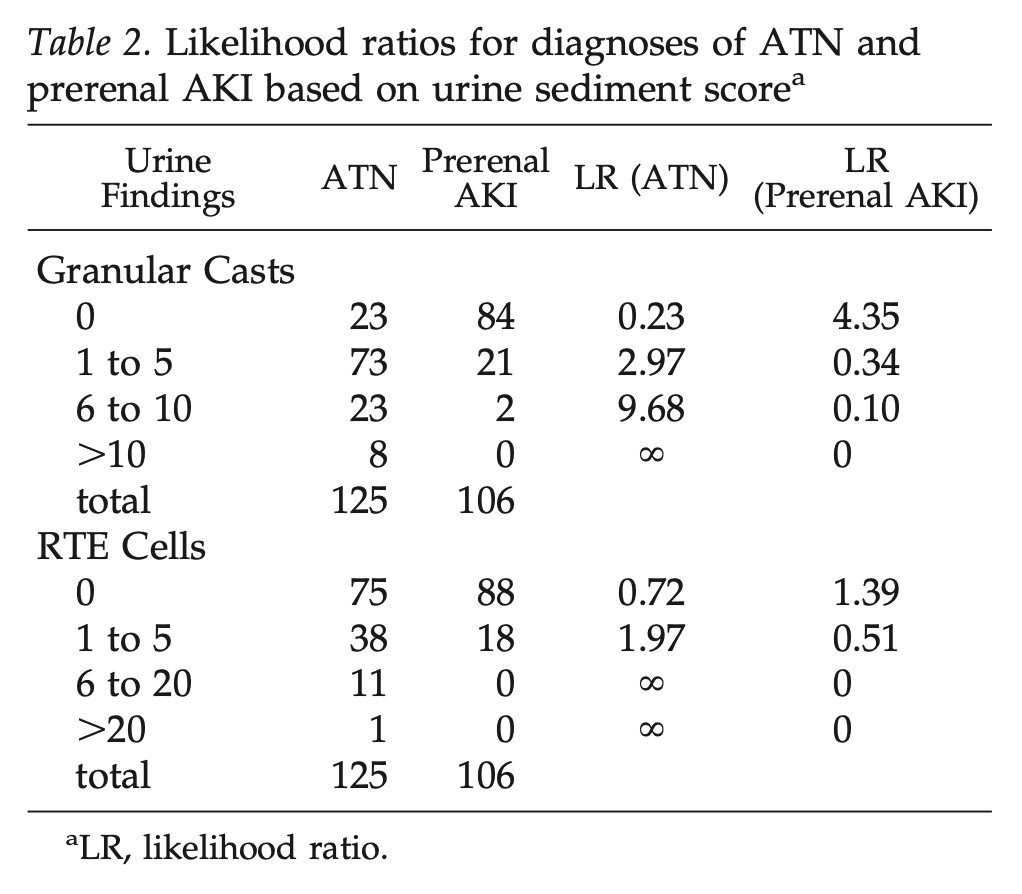
looked at the utility of urine microscopy in differentiating between prerenal AKI and ATN with impressive likelihood ratios from the presence or absence of granular casts/renal tubular epithelial cells
This paper:
 …https://cjasn-asnjournals-org.offcampus.lib.washington.edu/content/clinjasn/3/6/1615.full.pdf?with-ds=yes
…https://cjasn-asnjournals-org.offcampus.lib.washington.edu/content/clinjasn/3/6/1615.full.pdf?with-ds=yeslooked at the utility of urine microscopy in differentiating between prerenal AKI and ATN with impressive likelihood ratios from the presence or absence of granular casts/renal tubular epithelial cells
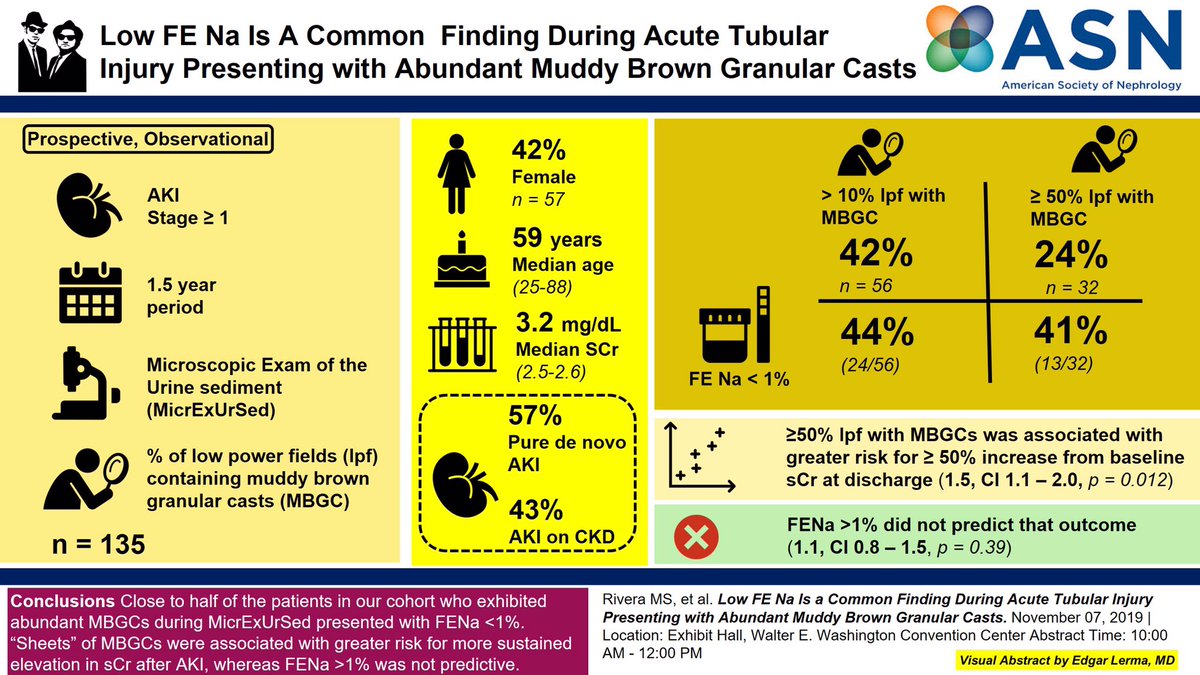
 This study found that a low FeNa (<1%) was common in patients with abundant muddy brown casts on microscopy.
This study found that a low FeNa (<1%) was common in patients with abundant muddy brown casts on microscopy. Image courtesy of @edgarvlermamd
Does this change your opinion?
The poll again:
To differentiate between prerenal AKI and ATN would you
The poll again:
To differentiate between prerenal AKI and ATN would you
Conclusion
 FeNa MAY be useful in highly selected patients if <1%
FeNa MAY be useful in highly selected patients if <1%
 >3% - who knows
>3% - who knows 
 Either way - shouldn't be ordered as a knee jerk in every patient with AKI
Either way - shouldn't be ordered as a knee jerk in every patient with AKI
 in these studies ATN/pre-renal were differentiated by rapidity of correction, often after volume repletion!
in these studies ATN/pre-renal were differentiated by rapidity of correction, often after volume repletion!
 FeNa MAY be useful in highly selected patients if <1%
FeNa MAY be useful in highly selected patients if <1% >3% - who knows
>3% - who knows 
 Either way - shouldn't be ordered as a knee jerk in every patient with AKI
Either way - shouldn't be ordered as a knee jerk in every patient with AKI in these studies ATN/pre-renal were differentiated by rapidity of correction, often after volume repletion!
in these studies ATN/pre-renal were differentiated by rapidity of correction, often after volume repletion!

 Read on Twitter
Read on Twitter