As promised @G_backlater ... my thoughts on this recent paper from @TheBJPsych ... https://twitter.com/g_backlater/status/1275483336161538051
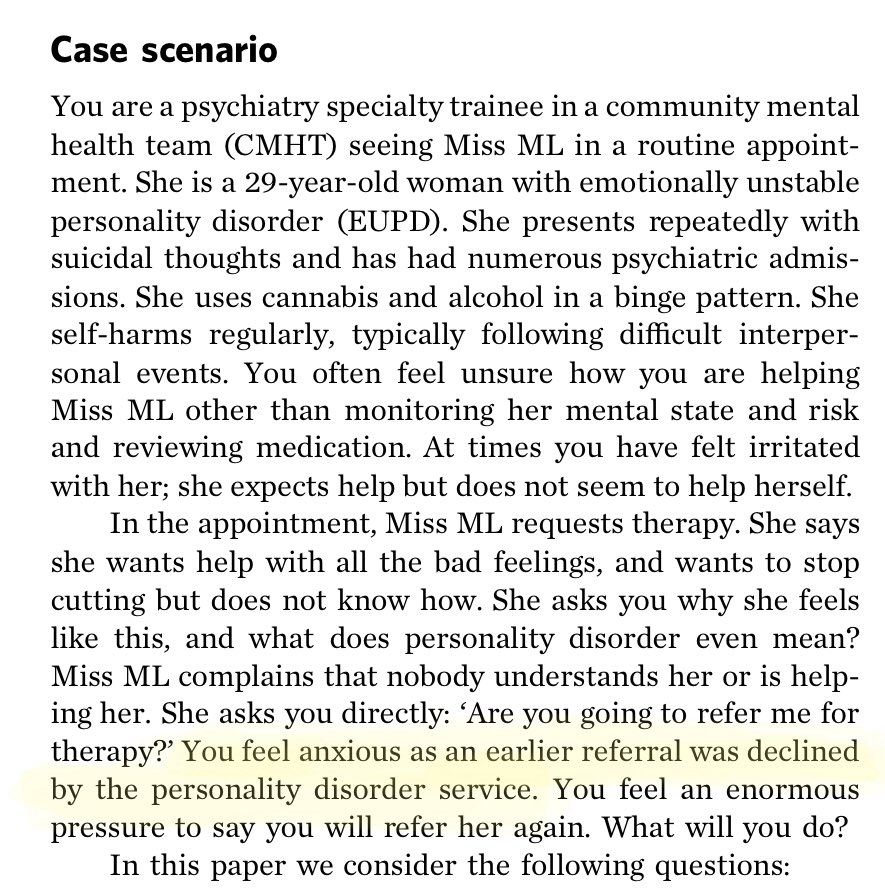
The paper highlights a common clinical problem - people with complex problems, suicidal thoughts, difficulties with substances with frequent admissions cared for in CMHT style settings can’t access psychological therapies & CMHT not doing much more than monitoring & prescribing
The staff are frustrated and getting irritated with the patient and the patient is frustrated and irritated by the care she is (or rather is not) receiving and the “personality disorder service” (most likely a psychological therapies service) is washing their hands of the issue
This is far from unusual... the nature of these problems (I tend towards the #traumanotPD school of thought) is that people struggling with them have intensely distressing emotions, use risky behaviours to cope, struggle with relationships & often face huge social difficulties...
So please, someone, explain to me why we should expect people to get better before treatment?
Another case...describing how it took years to become ready for therapy & for a joint meeting with the CMHT, alcohol service and personality disorder service was facilitated ( #traumanotPD) ...
Who took years to become ready for therapy? The patient? Or the services?
Who took years to become ready for therapy? The patient? Or the services?
Current guidelines don’t make any recommendations re how to increase “readiness for therapy” so the authors looked for literature on how to enhance “readiness for therapy” presumably to inform how CMHT clinician might help ppl in this predicament into psychological therapy
They found one study that looked at clinicians perspectives on what predicted poor engagement with therapy in a forensic population ... interesting but not necessarily immediately relevant here where the individual isn’t even given the chance to access therapy
Indeed... and that includes clinicians from specialist services when they set up tremendous barriers to accessing treatment
They mention a number ways CMHTs can help ppl (care coordination, continuity, safeguarding) and then some specific ways of helping ppl become more ready for therapy depending on where they might be considered to be on a stages for change model...
These inclu psychoeducation, formulation, goal setting, crisis planning, help with substance abuse, distress tolerance skills, addressing social situation, motivational interviewing, mindfulness, peer support, therapies that don’t rely on verbal communication & employment support
None of these have any evidence to support the idea they improve readiness to engage in therapy. With the exceptions of addressing social situations, peer support, alternative therapies and employment support...ALL of them are part and parcel of psychological therapies

The authors do note that the stages of change model has been used mainly to address single health behaviour rather than the complexity of problems experienced by patients in CMHTs...
Interestingly they didn’t suggest that services should change!
Should psychological therapies services be more flexible, more tolerant of disruptions in engagement, crises & complexity in therapy. Should we learn to roll with the “punches” & stick with patients?
Should psychological therapies services be more flexible, more tolerant of disruptions in engagement, crises & complexity in therapy. Should we learn to roll with the “punches” & stick with patients?
So I have 2 key thoughts here as someone who has primarily worked in CMHT, acute inpatient settings and private practice ...
The thread broke ... apologies... this tweet should link to this one: https://twitter.com/ruthannharpur/status/1275722739932893184?s=21

 Read on Twitter
Read on Twitter