On its face (and maybe even after some careful consideration), this article is concerning. The First Covid Vaccines May Not Prevent Covid Infection http://a.msn.com/00/en-us/BB15tVS8?ocid=st
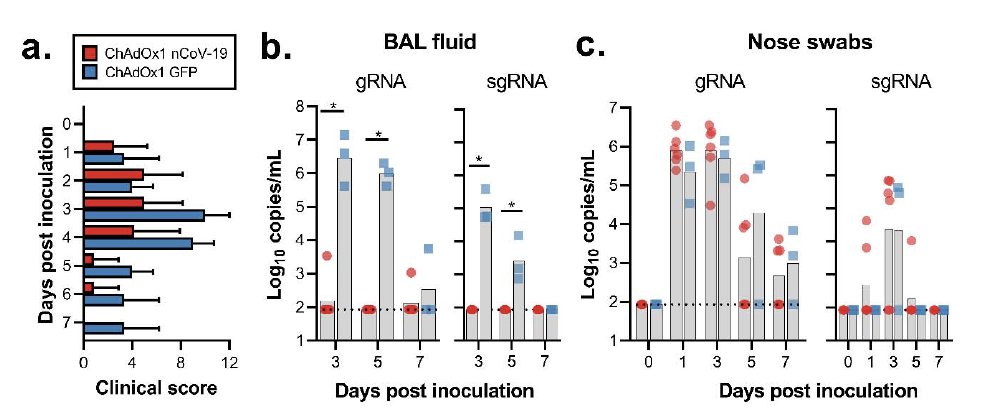
It points out as as been noted before https://blogs.sciencemag.org/pipeline/archives/2020/05/18/criticism-of-the-oxford-coronavirus-vaccine that the Oxford vaccine in macaque studies does not prevent (or even visibly reduce) the nasal shedding of virus RNA -- infection and perhaps contagiousness are the same, but vaccinated macaques don't get sick
and have much less virus RNA in their lungs
(from https://www.biorxiv.org/content/10.1101/2020.05.13.093195v1.full.pdf) -- concern originated with Bill Haseltine https://www.forbes.com/sites/williamhaseltine/2020/05/16/did-the-oxford-covid-vaccine-work-in-monkeys-not-really/#59d33e623c71
(from https://www.biorxiv.org/content/10.1101/2020.05.13.093195v1.full.pdf) -- concern originated with Bill Haseltine https://www.forbes.com/sites/williamhaseltine/2020/05/16/did-the-oxford-covid-vaccine-work-in-monkeys-not-really/#59d33e623c71
If true of any vaccine, this will be very unfortunate. Reduction in the risk of infection -- and onward transmission -- is the basis of herd immunity. A vaccine that protects against disease but not infection or transmission would help recipients but not the rest of us.
Herd immunity matters for COVID vaccines for several reasons -- most importantly, it will make a given number of vaccines provide more benefit -- as with nearly all other vaccines -- as vaccinating some reduces transmission to others
Those others may not get a vaccine (because of limited supply or other reasons) or it may not work as well in them (as many vaccines, for example don't work as well in the elderly).
Compounding this challenge will be that trials will be designed and powered, per the Bloomberg report, to see reductions in disease, with infection as a 2dary endpoint. We have suggested some ways to improve such trials to measure both ( @rebeccajk13 et al) https://academic.oup.com/aje/article/188/2/467/5134102
It comes down to getting good serological samples on participants before and after the trial, and being able to tell vaccine immunity from naturally acquired immunity to infection (should be possible for nearly all SARS-CoV-2 vaccines) https://www.nature.com/articles/s41591-020-0887-3
But I think there is also a more optimistic perspective - these vaccines may work better in humans in the field than in macaques in the lab -- for reasons of exposure dose, an often-forgotten variable as @mgmgomes1 has been arguing for years https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1003849
When you do an experimental infection, especially with precious animals in the lab like macaques, you typically look for a "challenge" dose that is high enough so that nearly all challenged animals will get infected, if not vaccinated.
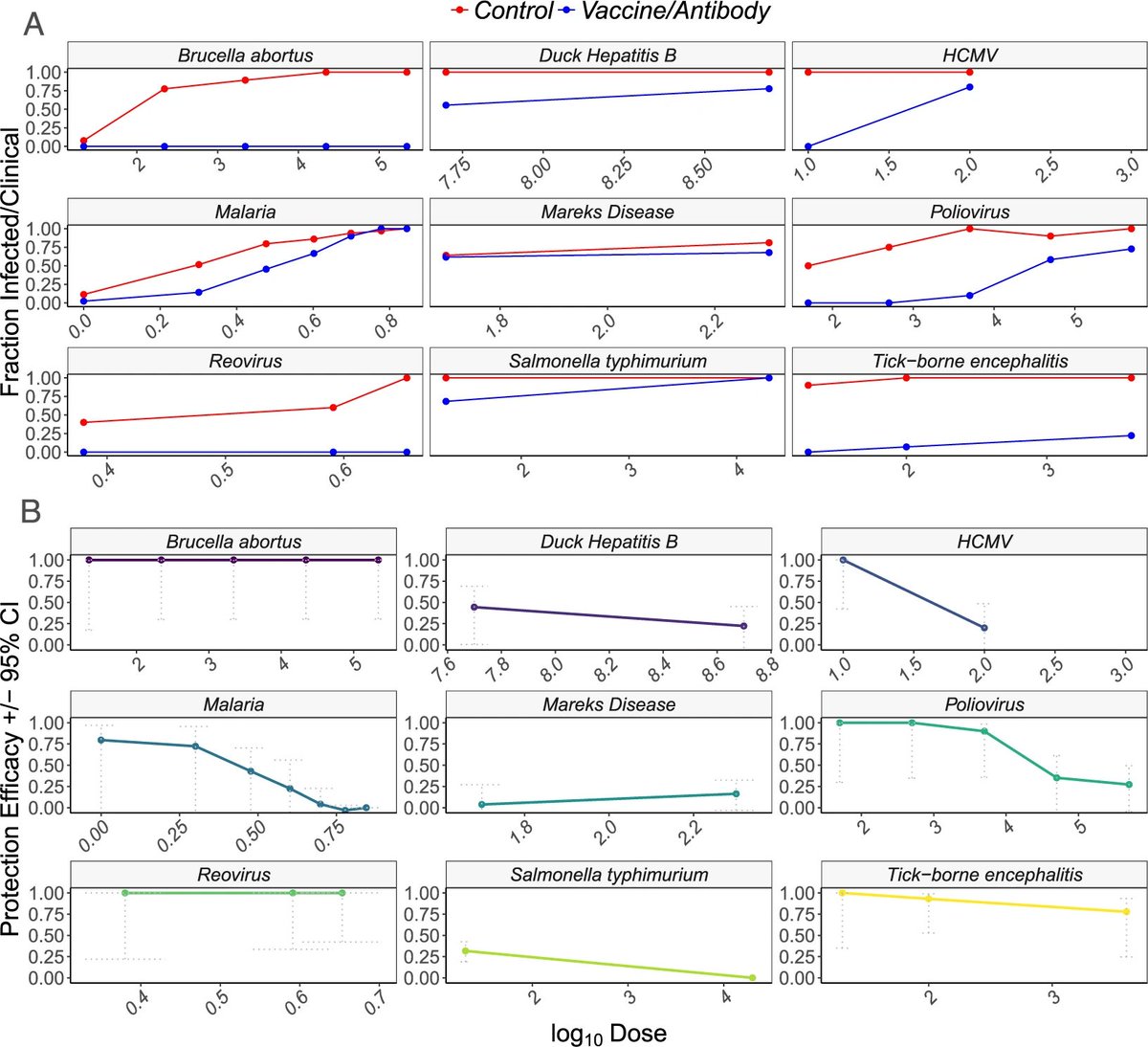
With @ecoevo_kel @mgmgomes1 and others, we looked at existing vaccine studies in animals to test the theoretical prediction that vaccines would be less efficacious when confronted with a large challenge dose https://www.nature.com/articles/s41598-019-39698-x.
The limited data we could find -- for a range of bacterial and viral pathogens -- was consistent with this expectation.
So there are grounds to hope -- either because macaques are different from humans and/or because the typical dose to which a person is exposed is lower, and the vaccine may work better at such doses, that humans will be at least partially protected vs infection/contagiousness
The same considerations apply to other vaccines. Bottom line -- while getting some answer about vaccine efficacy is extremely urgent, understanding its effects on infection/infectiousness and knowing if it works well in elderly will be crucial to planning how to deploy a vaccine.
As ever, @HelenBranswell has good points to add. First that she had pointed all this out a month ago! (she said it far more politely, but I am not Canadian so I'm saying it bluntly) https://www.statnews.com/2020/05/22/the-world-needs-covid-19-vaccines-it-may-also-be-overestimating-their-power/. Second, that a post-vax infection could create full immunity w/o disease
though as was pointed out in reply to my thread earlier, this person would still potentially transmit while acquiring the sterilizing immunity from the postvaccine infection
Related to all this: the household secondary attack rate in most studies seems to be 10-15% ballpark. Can we distinguish between 1) the typical dose experienced by a household member has only a 3% (say - if 5 days of exposure once a day) chance of infecting them vs.
2) the typical dose experienced by a household member is very likely (>50%) to infect them, and most household members don't actually inhale or otherwise potentially infect themselves with any virus shed by the index?

 Read on Twitter
Read on Twitter