Great and important that new original research is being performed on longstanding groin pain in athletes (but I might be a bit biased). Apart from terminology preferences, conducting and interpreting diagnostic accuracy studies in longstanding groin is challenging IMO 1/n https://twitter.com/kcrehabexpert/status/1272954062376443906
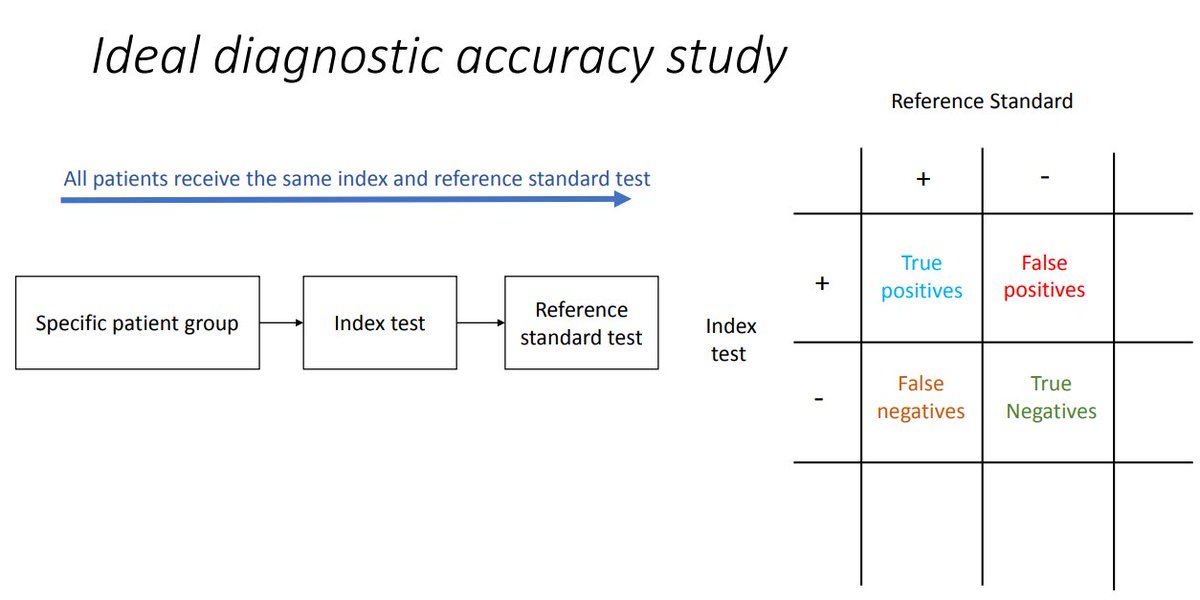
In a diagnostic accuracy study, we ideally want to compare index test(s) with a:
 gold standard (=error-free reference standard)
gold standard (=error-free reference standard)
 OR, a best available reference standard for establishing the presence or absence of the target condition.
OR, a best available reference standard for establishing the presence or absence of the target condition.
https://ebm.bmj.com/content/23/2/54 2/n
 gold standard (=error-free reference standard)
gold standard (=error-free reference standard) OR, a best available reference standard for establishing the presence or absence of the target condition.
OR, a best available reference standard for establishing the presence or absence of the target condition.https://ebm.bmj.com/content/23/2/54 2/n
In longstanding groin pain in athletes:
 there is no accepted gold standard.
there is no accepted gold standard.
 imaging findings (MRI/US) are often (false) positive in a-symptomatic athletes, making it's utility as reference standard currently debatable.
imaging findings (MRI/US) are often (false) positive in a-symptomatic athletes, making it's utility as reference standard currently debatable.
https://bjsm.bmj.com/content/49/10/681.long
https://pubmed.ncbi.nlm.nih.gov/24603080/ 3/n
 there is no accepted gold standard.
there is no accepted gold standard.  imaging findings (MRI/US) are often (false) positive in a-symptomatic athletes, making it's utility as reference standard currently debatable.
imaging findings (MRI/US) are often (false) positive in a-symptomatic athletes, making it's utility as reference standard currently debatable.https://bjsm.bmj.com/content/49/10/681.long
https://pubmed.ncbi.nlm.nih.gov/24603080/ 3/n
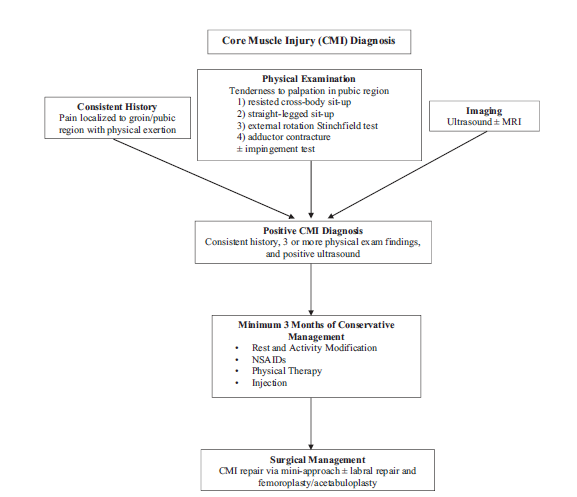
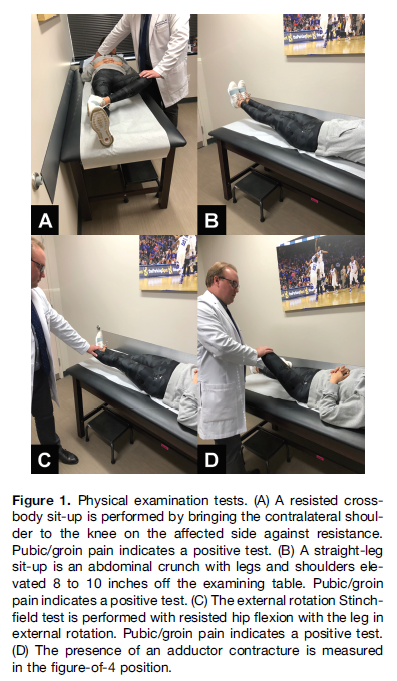
The purpose of this AJSM study( https://journals.sagepub.com/doi/abs/10.1177/0363546520926029) was: "to determine the diagnostic accuracy of various physical examination tests in the diagnosis of CMI". MRI was used as a reference standard (although in the algorithm also an index test and not a reference standard )4/n
)4/n
 )4/n
)4/n
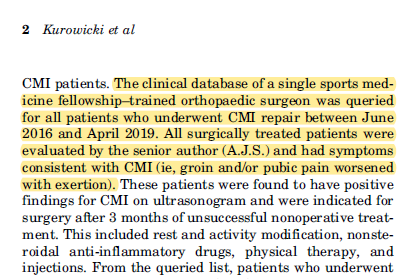
Patients (n=81) were (retrospectively) recruited from a database where all underwent "CMI repair". I.e. all included patients were "CMI" diagnosed patients and thus probably had 3 or more positive physical exam findings according to the presented algorithm. 5/n
5/n
 5/n
5/n
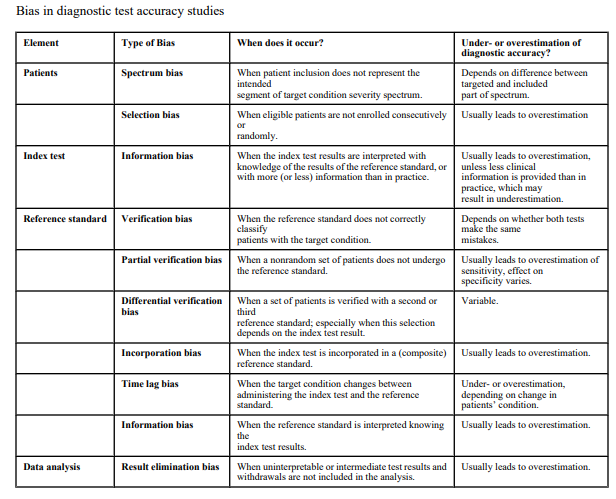
If the index test is part of the reference standard - which is often the case in diagnostic accuracy studies in longstanding groin pain - there is a high risk of incorporation bias ( usually causes overestimation test results)
usually causes overestimation test results)
https://www.acpjournals.org/doi/10.7326/0003-4819-149-12-200812160-00008 6/n
 usually causes overestimation test results)
usually causes overestimation test results)https://www.acpjournals.org/doi/10.7326/0003-4819-149-12-200812160-00008 6/n
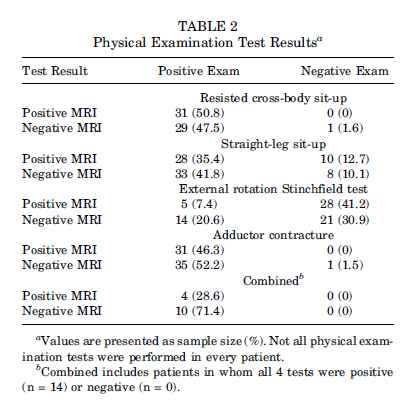
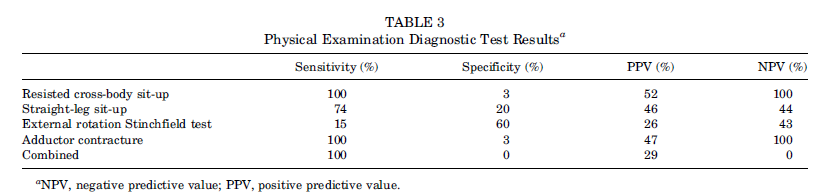
Thus, for this @AJSM_SportsMed study, if 3 of 4 investigated clinical examination tests had to be positive for the diagnosis "CMI", most likely there will be a high prevalence (and sensitivity) of positive tests and subsequent high risk of incorporation bias. 7/n
Fortunately, the authors transparently reported their results which shows that "resisted cross-body sit-up" and "adductor contracture" tests are positive in all(!) (but 1) cases  unsurprisingly, combining the test results, gives sens 100%/spec 0% 8/n
unsurprisingly, combining the test results, gives sens 100%/spec 0% 8/n
 unsurprisingly, combining the test results, gives sens 100%/spec 0% 8/n
unsurprisingly, combining the test results, gives sens 100%/spec 0% 8/n
IMO, these results need careful interpretation:
 only "positive CMI cases" included (selection bias)
only "positive CMI cases" included (selection bias)
 unknown reliability of presented clinical exam tests
unknown reliability of presented clinical exam tests
 unclear/unreliable reference standard
unclear/unreliable reference standard
 index tests were part of reference standard (incorporation bias)
index tests were part of reference standard (incorporation bias)
9/n
 only "positive CMI cases" included (selection bias)
only "positive CMI cases" included (selection bias) unknown reliability of presented clinical exam tests
unknown reliability of presented clinical exam tests unclear/unreliable reference standard
unclear/unreliable reference standard index tests were part of reference standard (incorporation bias)
index tests were part of reference standard (incorporation bias) 9/n
I want to emphasize that I'm acknowledging the hard work and best intentions of the authors, because we often want to answer our clinical questions and improve knowledge for the field with limited resources available (and this is hard work for researchers) 10/n
However, I wanted to respectfully highlight the limitations of this study results IMO (in a high impact journal) and the challenges of diagnostic accuracy studies in longstanding groin pain in general. 11/n
Taking 1 step back - we might want to focus (first) on further developing well defined and reliable clinical examination tests and imaging findings, and subsequently investigate their relation with outcomes (prognosis/treatment). 12/n https://bjsm.bmj.com/content/38/4/446.long
If we want to conduct a diagnostic accuracy study in longstanding groin pain, we probably must accept that there will be biases/limitations. There are some solutions to reduce these biases by following recommendations.
https://bmjopen.bmj.com/content/6/11/e012799
https://www.journalslibrary.nihr.ac.uk/hta/hta11500#/abstract 13/end
https://bmjopen.bmj.com/content/6/11/e012799
https://www.journalslibrary.nihr.ac.uk/hta/hta11500#/abstract 13/end

 Read on Twitter
Read on Twitter