1) The responsibility for health and wellbeing in local government is not new but has a long and prestigious history. From the Victorian Public Health Acts, it was local government that held the principal responsibility for the health and wellbeing of their populations.
2) Improving health in Victorian times concentrated on developments in sanitation, living and working conditions, and tackling infectious diseases. Local government was clearly best placed to do this and has continued to lead in these areas
3) Local govts long history can still be seen reflected in the mottos of several English councils, Salus populi suprema lex, translated as “The health and welfare of the people should be the highest law”.
4) Southwark Council translated the phrase into English and carved out in bricks and mortar and placed it proudly above the entrance of the new Walworth Clinic opened in 1937.
It is also the moto of Borough of Lewisham and Salford Council in Greater Manchester
It is also the moto of Borough of Lewisham and Salford Council in Greater Manchester
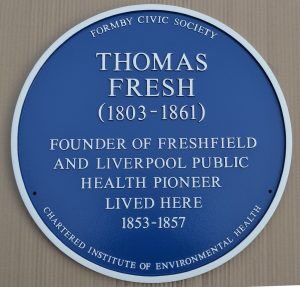
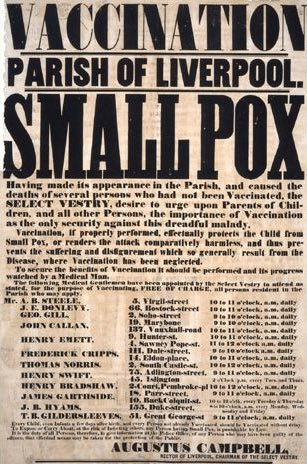
5) Thomas Fresh was Liverpool’s first public health officer, having been appointed Inspector of Nuisances by the Health of Towns Committee in 1844. He is often cited as the first environmental health practitioner.
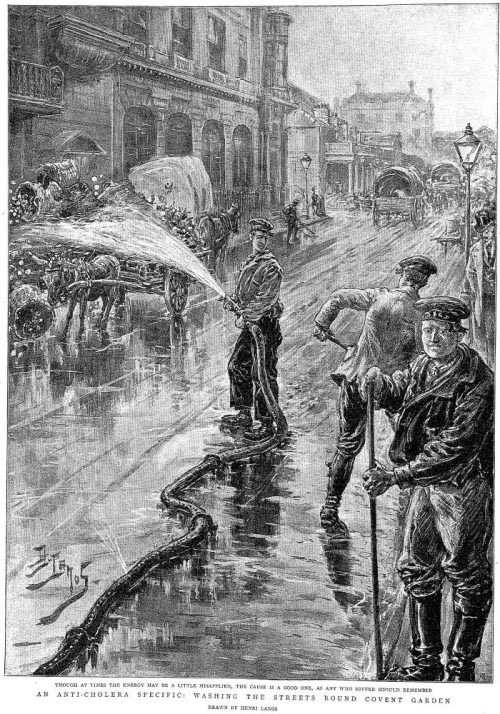
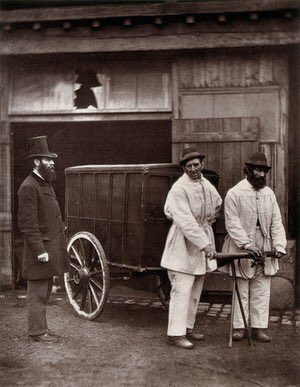
6) Inspectors of Nuisances were the forefathers of today's environmental health practitioners.  The top-hatted man supervising was Mr. Dickson, Inspector of Nuisances for the parish of St. George, Hanover Square.
The top-hatted man supervising was Mr. Dickson, Inspector of Nuisances for the parish of St. George, Hanover Square.
 The top-hatted man supervising was Mr. Dickson, Inspector of Nuisances for the parish of St. George, Hanover Square.
The top-hatted man supervising was Mr. Dickson, Inspector of Nuisances for the parish of St. George, Hanover Square.
7) In 1848 the first Public Health Act caused the setting up of a Board of Health, and gave towns the right to appoint a Medical Officer of Health and in 1853 vaccination against smallpox was made compulsory.
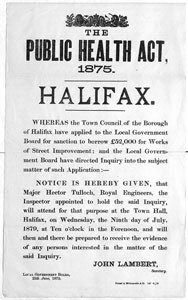
8) After the 1867 Improvement Act it was possible for local authorities to take out loans at favourable rates to develop services. Regulations governing LA borrowing were a major factor in the financing of sewers and the level of investment in sewage disposal rose dramatically.
9) In Birmingham under Joseph Chamberlain who was Mayor of the city from 1873 to 1875, provision was made for gas and water supplies. They also cleared slums and introduced a city park system. These reforms were designed to better the lives of the people of Birmingham.
10) When asked about the cost, Chamberlain said,
‘We have not the slightest intention of making profit…We shall get our profit indirectly in the comfort of the town and in the health of the inhabitants’.
‘We have not the slightest intention of making profit…We shall get our profit indirectly in the comfort of the town and in the health of the inhabitants’.
The Public Health Act of 1875 meant that every public health authority had to have a medical officer and a sanitary inspector, to ensure the laws on food, housing, water and hygiene were carried out; and that towns had to have pavements and street lighting.
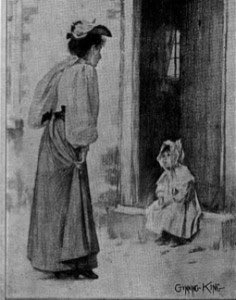
12) Councils like Liverpool pioneered many of the developments that have taken place in public health over the past two centuries. In the late nineteenth century the city was one of the first to provide a health visiting service, mother and infant welfare centres,
13) The first health visitors employed by a LA developed from the role of ladies’ sanitary inspector and were known as ‘sanitary visitors’. The role was primarily to promote health and to provide health education, working at the level of the infant, their family and the community
14) From 1837, civil registration of deaths gave local policymakers data on rates of mortality by age, sex, cause and place. As a result of the Births and Deaths Act 1874, the onus was on parents to inform the registrar when they had a child and penalties imposed on transgressors
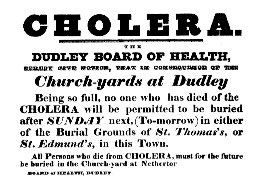
15) The statutory requirement for the notification of certain infectious diseases first came into being with the Infectious Disease (Notification) Act 1889, which made reporting compulsory in London and optional elsewhere.
16) Cases of smallpox, cholera, diphtheria, scarlet fever, typhus fever, typhoid fever, enteric fever had to be reported by the household head or attending doctor to the local authority. The system spread to the rest of England and Wales in 1899.
17) Householders who failed to notify a case of one of these diseases was liable to a fine of up to forty shillings. The local sanitary authority could pursue existing public health laws to isolate patients in hospital, disinfect property, suspend schooling and close businesses.
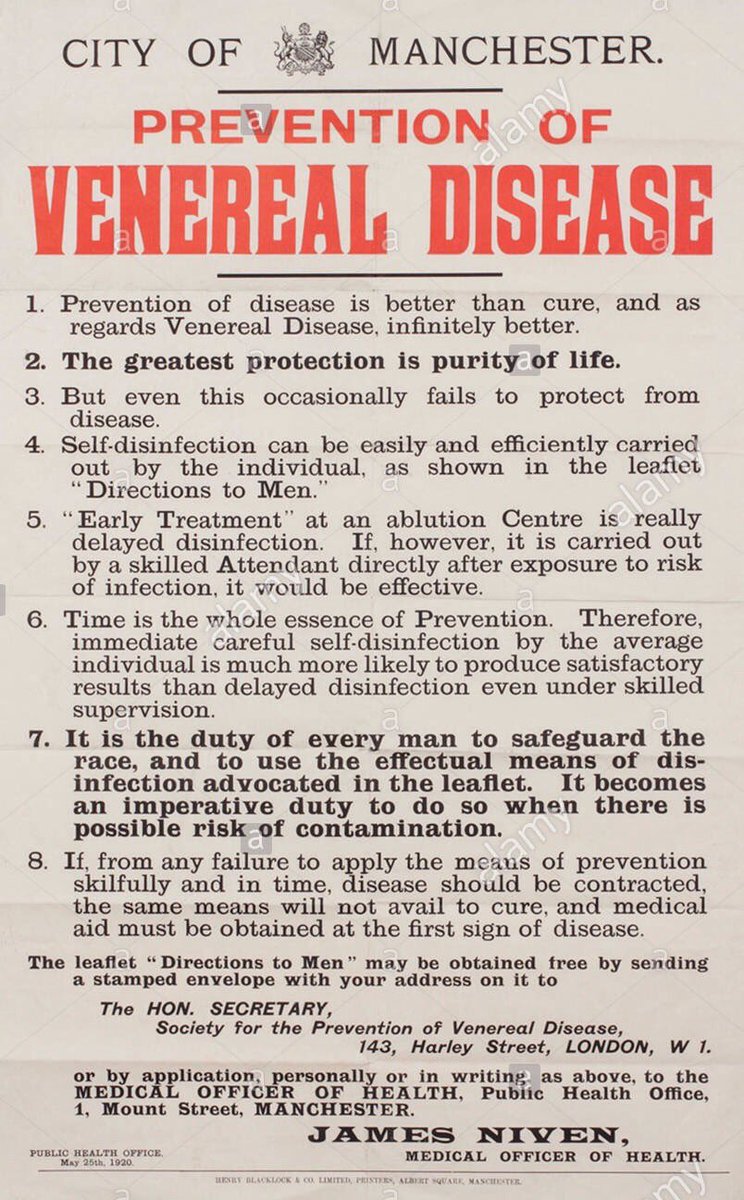
18) In July 1916, the Local Government Board issued the Public Health (Venereal Diseases) Regulations. This began the process of providing free, confidential diagnosis and treatment for sexually transmitted infections (STIs). In May 1917, the Venereal Disease Act was passed.
19) During the first world war about 5% of men in Britain’s armies were infected with an STI and over 400,000 British or allied troops were admitted to hospital due to a sexual infection.
20) The statutory provision of school nursing in all schools in the UK arose out of the need to improve the health of children living in poverty and this coincided with the Boer War. A large proportion of army volunteers had been found to be medically unfit for service.
21) In 1903, the government set up the Interdepartmental Committee on Physical Deterioration to study the causes. The government reacted to the findings of the report by passing the 1906 Provision of School Meals Act which allowed LAs to provide school meals for the poor.
22) The 1907 Education Act established a team of school nurses at every local authority. This was accompanied by the 1907 Medical Inspections Act, which required LAs to ensure that each child received a total of at least 3 medical inspections during their time at school.
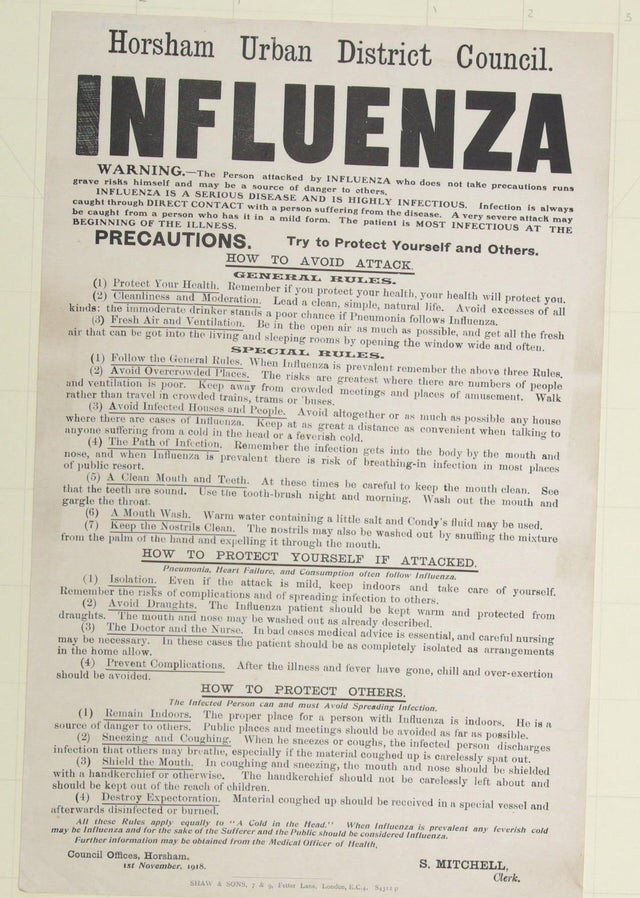
23) The Spanish flu pandemic of 1918, the deadliest in history, infected an estimated 500 million people worldwide—about one-third of the planet’s population. One out of every 30 people died. The outbreak claimed the lives of nearly 250,000 Britons.
24) The first wave of the Spanish flu struck in the spring of 1918. The majority of victims were adults aged 20 to 40 – the inverse of most flu seasons, when deaths fall most heavily on the elderly. Schools were closed, public gatherings banned and people encouraged to wear masks
25) What is often missed, is the important role of local authorities. In some areas, they ran and owned the hospitals, kept essential services running – such as mortuaries, burials, shelters, food distribution, care for people left without carers or children without parents.
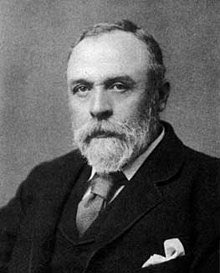
26) Dr James Niven, medical officer for Manchester at the time, was the first to introduce preventative measures that slowed the spread of the disease, saving many lives. Niven recognised earlier on the nature of this pandemic and how it could easily be spread through the city.
27) Niven reccommended that schools and cinemas be closed to reduce people's proximity to each other and published leaflets that were displayed around the city, advising residents on how to reduce the risk of becoming infected. His saying was said to be “spit kills”.
28) Niven meticulously analysed statistics to be as informed as he could be so that he could give the people of Manchester the best advice. He said at the time: "Public health authorities should press for further precautions in the presence of a severe outbreak."
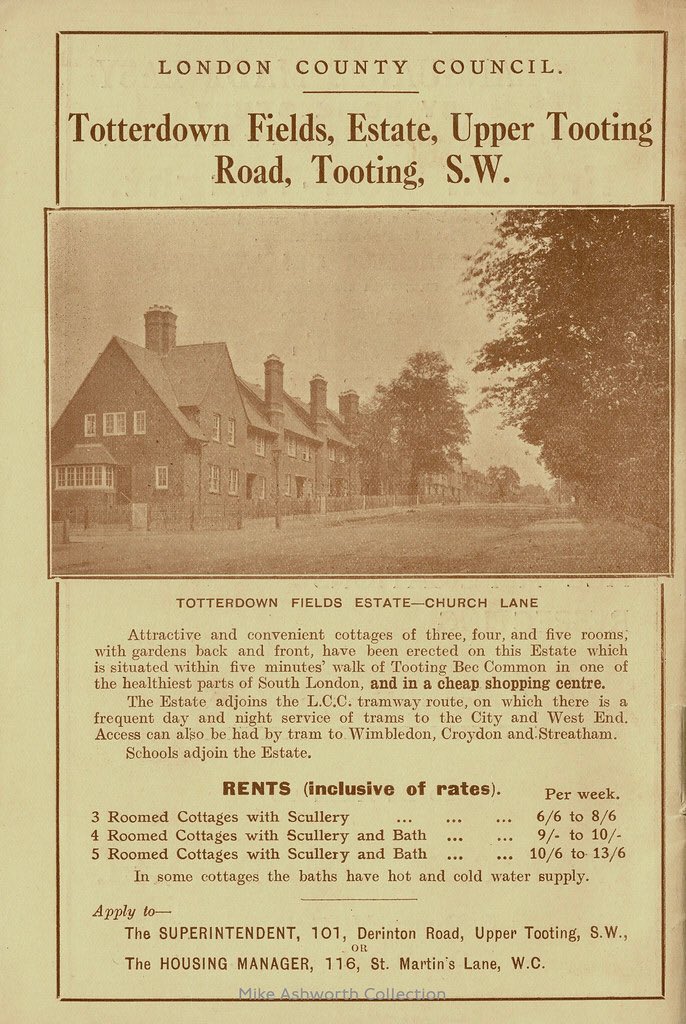
29) The end of the First World War in 1918 created a huge demand for working-class housing in towns throughout Britain. In 1919, Parliament passed the ambitious Housing 'Addison' Act, named after its author, Dr Christopher Addison, the Minister of Health
30) It made housing a national responsibility, and local authorities were given the task of developing new housing and rented accommodation where it was needed. The Housing Act 1924 gave substantial grants to local authorities in response to the acute housing shortages.
31) A fresh Housing Act of 1930 obliged local councils to clear all remaining slum housing, and provided further subsidies to re-house inhabitants. This single Act led to the clearance of more slums than at any time previously, and the building of 700,000 new homes.
32) Under the provisions of the inter-war Housing Acts local councils built a total of 1.1 million homes.
33) At the beginning of 20th century tuberculosis was one of the biggest killers in the UK, responsible for more deaths than any other disease. The TB bacterium usually attack the lungs, but TB bacteria can attack any part of the body such as the kidney, spine, and brain.
34) During the 1920s one in every ten deaths in Northumberland was caused by TB, the County Council used around 75% of their health expenditure to tackle the disease.
In 1921 the Public Health (Tuberculosis) Act required local authorities make adequate provision for sanatoria treatment of tuberculosis, care and after-care services for tuberculosis patients.
36) In 1920, the first human trials of the vaccine Bacille Calmette-Guérin (BCG), are launched. In 1953, A survey of 50,000 children showed an 80% reduction in infection rate following the BCG vaccination, leading to its introduction in secondary schools in the UK until 2005.
37) During the 1950s, smog (a toxic combination of soot and sulphur dioxide) was commonplace in UK cities and a major source of disease. In 1952, the Great Smog of London killed more than 4,000 in the immediate aftermath, and a further 8,000 died in following weeks and months.
38) The Great Smog of 1952 was a pea-souper of unprecedented severity, induced by both weather and pollution. On December 5, an anticyclone settled over London, a high-pressure weather system that caused an inversion whereby cold air was trapped below warm air higher up.
39) Consequently, the emissions of factories and domestic fires could not be released into the atmosphere and remained trapped near ground level. The result was the worst pollution-based fog in the city’s history.
40) The Clean Air Acts of 1956 and 1968 were introduced to deal with the smog’s. The Acts gave local authorities powers to control emissions of dark smoke, grit, dust and fumes from industrial premises and furnaces and to declare "smoke control areas".

 Read on Twitter
Read on Twitter