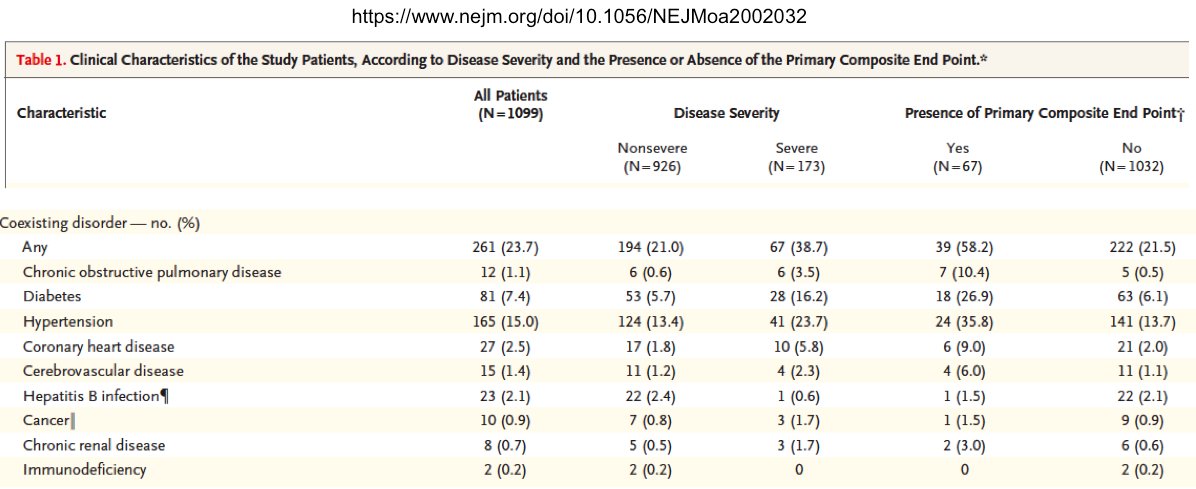
1 approach to understanding #covid19 infection is to examine co-morbidities & ask what's common?
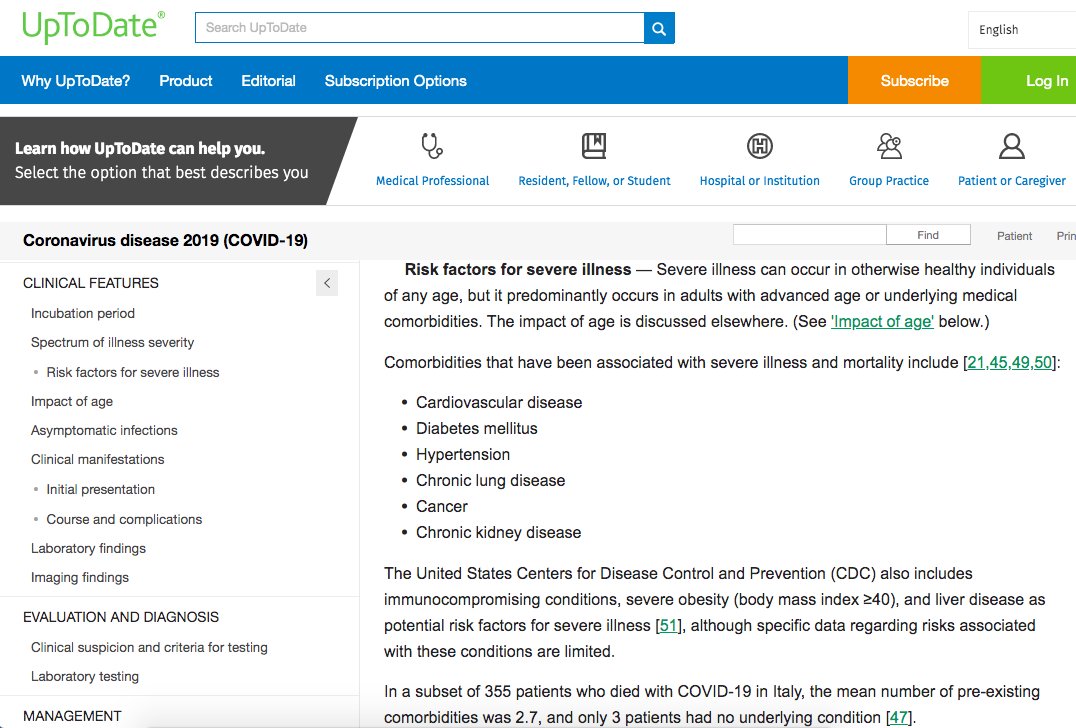
Most prevalent Cov19 co-morbs:
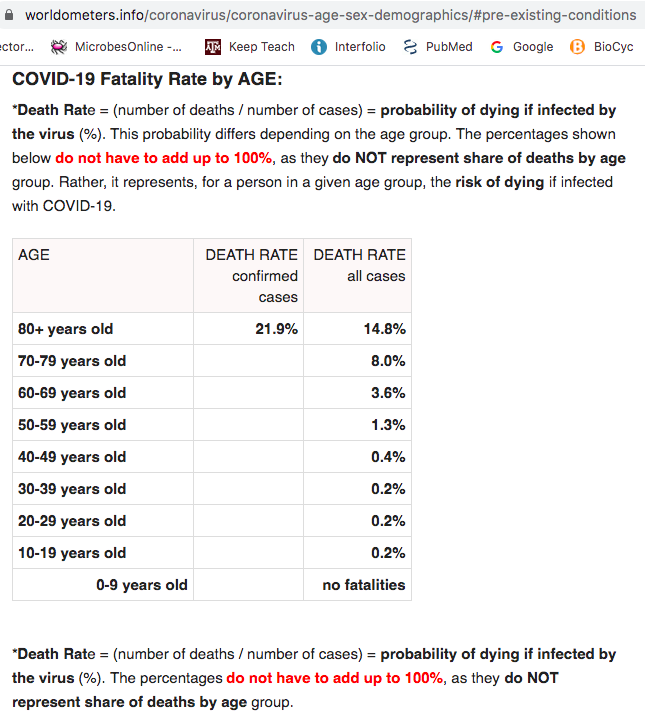
1) age
age
2)Hypertension
3)Diabetes
4)Cardiovascular disease
5)Kidney disease
6)Chronic respiratory disease (esp COPD)
8)Cancers
9)BMI>40
10) >
>
Most prevalent Cov19 co-morbs:
1)
 age
age2)Hypertension
3)Diabetes
4)Cardiovascular disease
5)Kidney disease
6)Chronic respiratory disease (esp COPD)
8)Cancers
9)BMI>40
10)
 >
>
2/
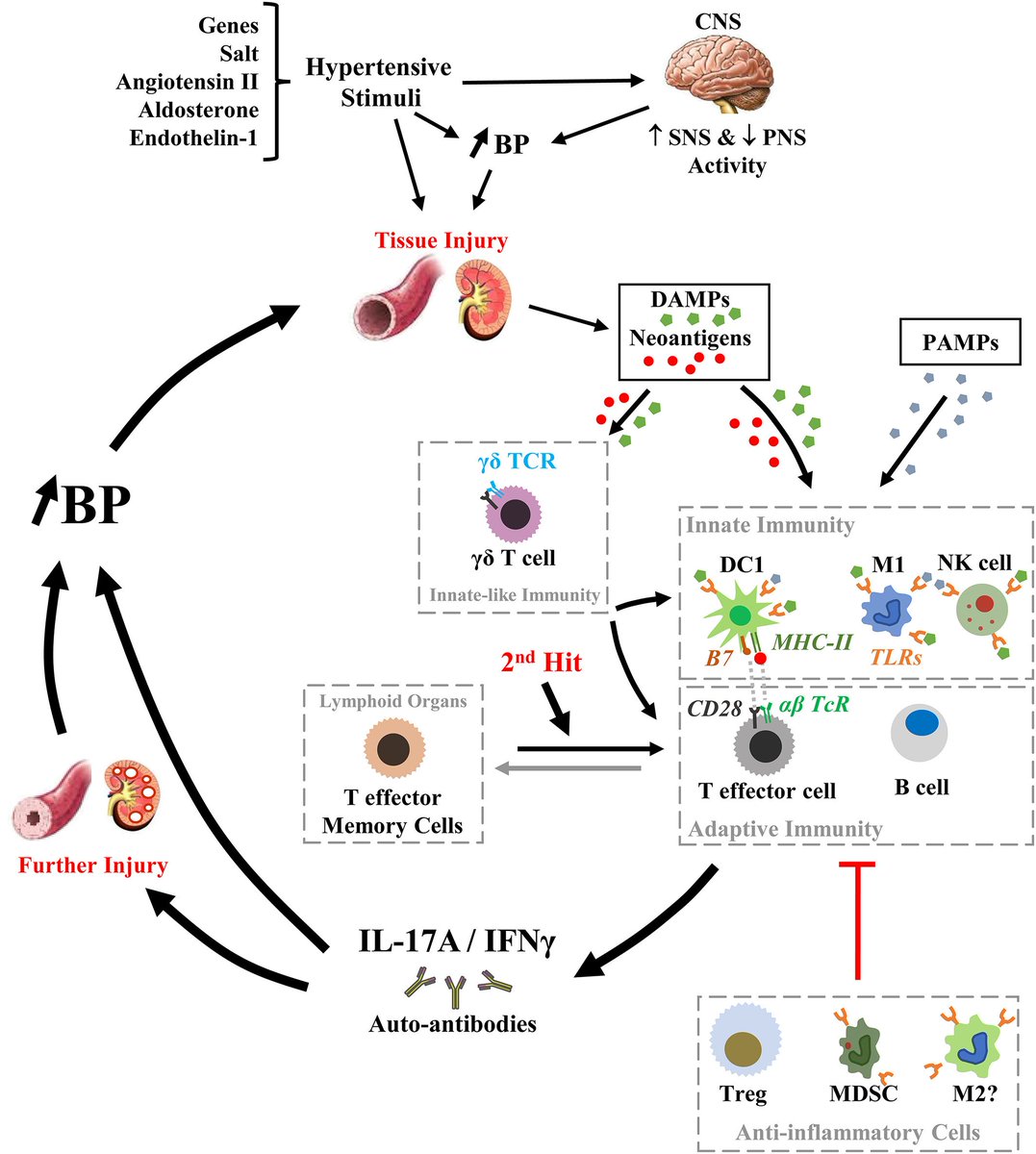
These are diverse diseases & increasing age technically not a disease at all. However, there is at least 1 factor in common among all of the co-morbidities identified thus far:
INFLAMMATION
These are diverse diseases & increasing age technically not a disease at all. However, there is at least 1 factor in common among all of the co-morbidities identified thus far:
INFLAMMATION
3/
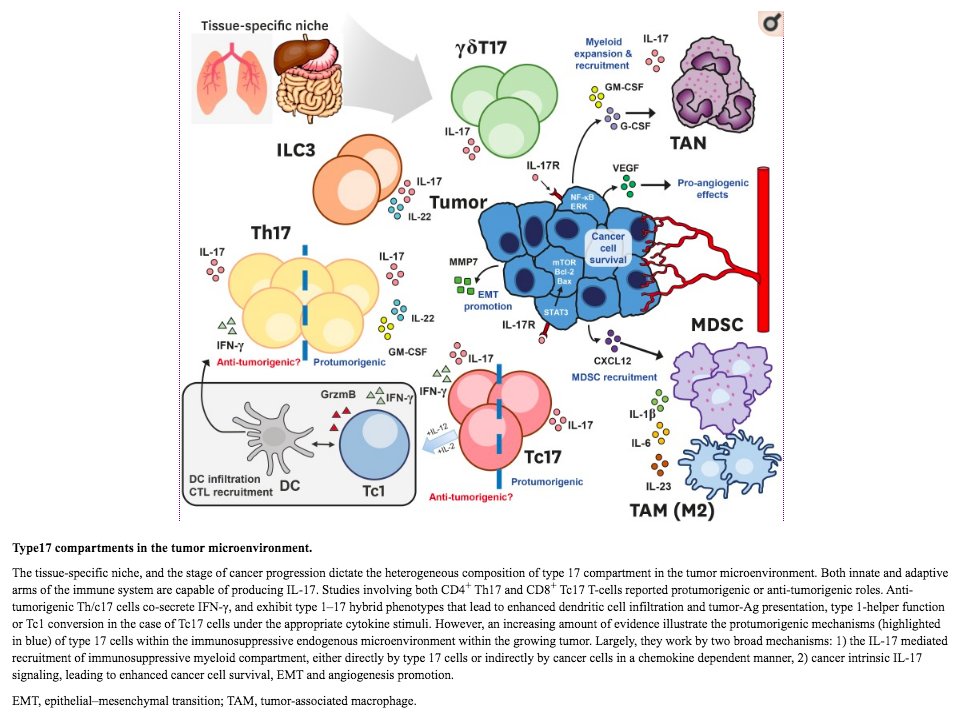
A survey of the co-morbidities revealed another commonality; a close association w/ dysregulation of the pro-inflammatory, neutrophil-recruiting cytokine, IL-17A.
IL-17A is made by multiple immune cell types, including lung-resident innate lymphoid cells (ILC3s).
A survey of the co-morbidities revealed another commonality; a close association w/ dysregulation of the pro-inflammatory, neutrophil-recruiting cytokine, IL-17A.
IL-17A is made by multiple immune cell types, including lung-resident innate lymphoid cells (ILC3s).
4/
While this isn't place for a comp review, I'll include 1+ reference highlighting relationship between IL-17A & each CoV19 co-morb.
Useful resources for info about IL-17A:
https://doi.org/10.4267/2042/55373
https://www.ncbi.nlm.nih.gov/pubmed/28254169
https://www.ncbi.nlm.nih.gov/pubmed/31745337
Also PMID 31337278 & 28620097
While this isn't place for a comp review, I'll include 1+ reference highlighting relationship between IL-17A & each CoV19 co-morb.
Useful resources for info about IL-17A:
https://doi.org/10.4267/2042/55373
https://www.ncbi.nlm.nih.gov/pubmed/28254169
https://www.ncbi.nlm.nih.gov/pubmed/31745337
Also PMID 31337278 & 28620097
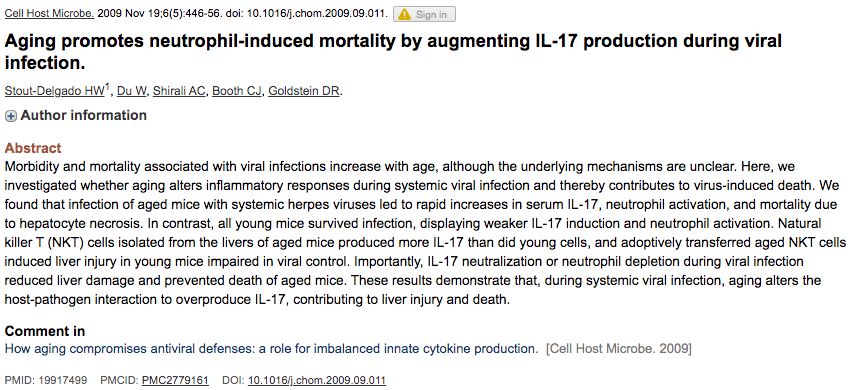
1) age
age
The increase inflammation that occurs with age (aka "inflammaging") is well-documented.
This paper shows how during viral infection, aged mice overproduce IL-17A (relative to young control), leading to neutrophil-mediated organ damage/death.
Rescued by anti-IL-17A Ab
 age
ageThe increase inflammation that occurs with age (aka "inflammaging") is well-documented.
This paper shows how during viral infection, aged mice overproduce IL-17A (relative to young control), leading to neutrophil-mediated organ damage/death.
Rescued by anti-IL-17A Ab
6/
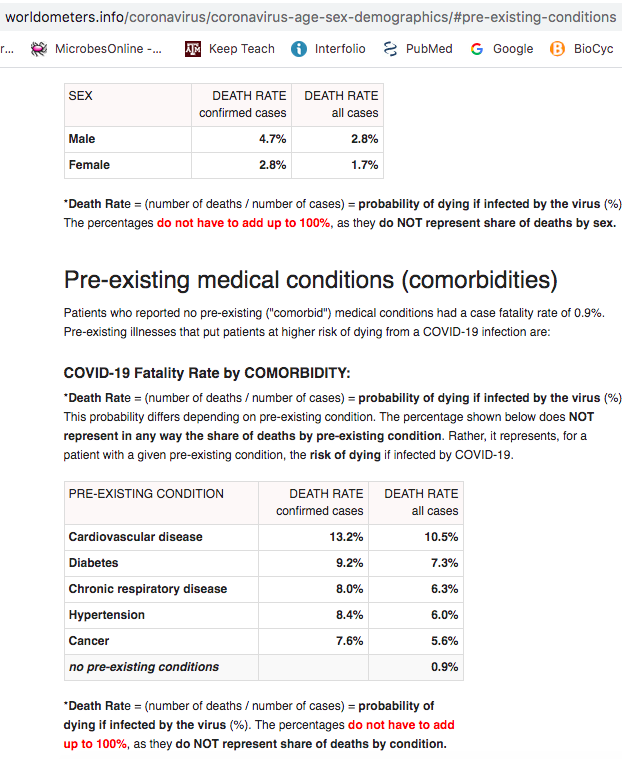
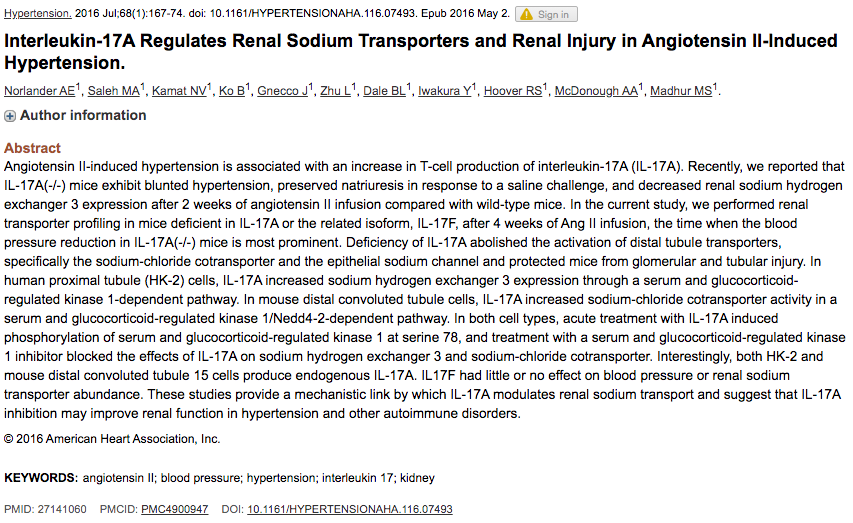
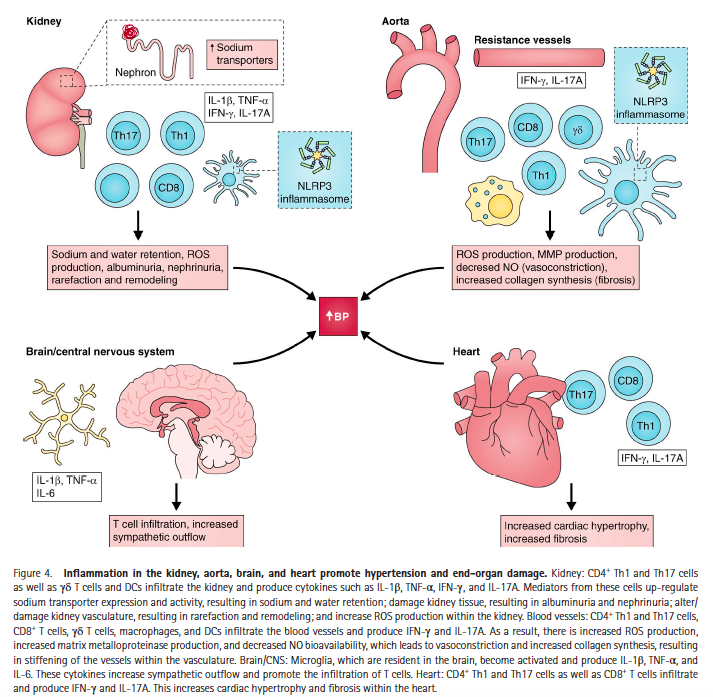
Close relationship of hypertension/kidney disease/diabetes, so some overlap in refs
2)hypertension
In short, Angiotensin II (produced by ACE) leads to elevated IL-17A & inflammation and hypertension. Targeting IL-17A lowers blood pressure.
PMID 29952002 (recent review)
Close relationship of hypertension/kidney disease/diabetes, so some overlap in refs
2)hypertension
In short, Angiotensin II (produced by ACE) leads to elevated IL-17A & inflammation and hypertension. Targeting IL-17A lowers blood pressure.
PMID 29952002 (recent review)
7/
3)Diabetes
Due to the close relationship between hypertension, obesity, kidney disease, & diabetes, unclear if this is a separate co-morbidity.
Increased IL-17A is associated with secondary diabetic diseases and anti-IL-17A antibodies are being considered as therapeutics
3)Diabetes
Due to the close relationship between hypertension, obesity, kidney disease, & diabetes, unclear if this is a separate co-morbidity.
Increased IL-17A is associated with secondary diabetic diseases and anti-IL-17A antibodies are being considered as therapeutics
8/
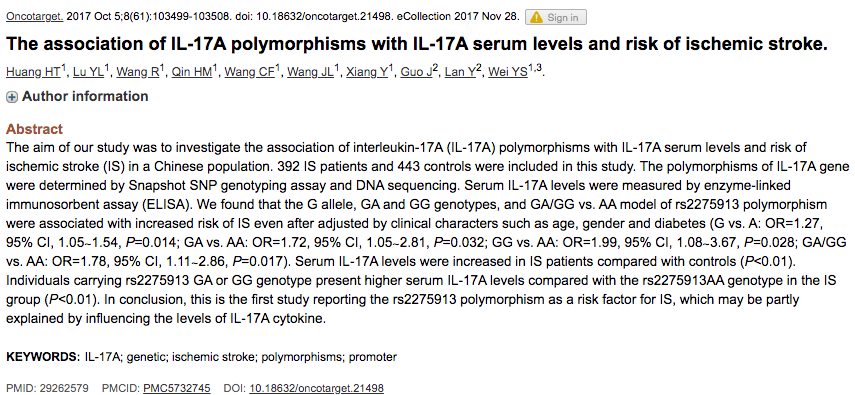
4) Cardiovascular disease
This co-morbidity should perhaps be classified as vascular disease; Chinese CoV19 patients were much more likely to have cerebrovascular disease than CV disease.
Also, overlap with hypertension. This is an older review.
4) Cardiovascular disease
This co-morbidity should perhaps be classified as vascular disease; Chinese CoV19 patients were much more likely to have cerebrovascular disease than CV disease.
Also, overlap with hypertension. This is an older review.
9/
5)Kidney disease
Impossible to decouple from hypertension - see /6
5)Kidney disease
Impossible to decouple from hypertension - see /6
10/
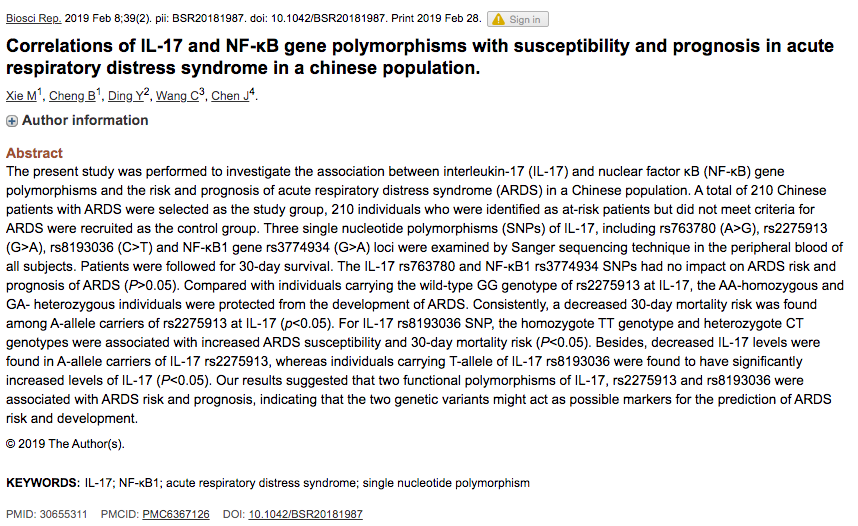
6)Chronic respiratory disease (esp COPD)
COPD & neutrophilic asthma have much in common. For both, IL-17A levels are elevated in BAL, implicated in pathology, & anti-IL-17A is being explored as a therapeutic
PMID 30383540/20565710/32172346 and many more
6)Chronic respiratory disease (esp COPD)
COPD & neutrophilic asthma have much in common. For both, IL-17A levels are elevated in BAL, implicated in pathology, & anti-IL-17A is being explored as a therapeutic
PMID 30383540/20565710/32172346 and many more
11/
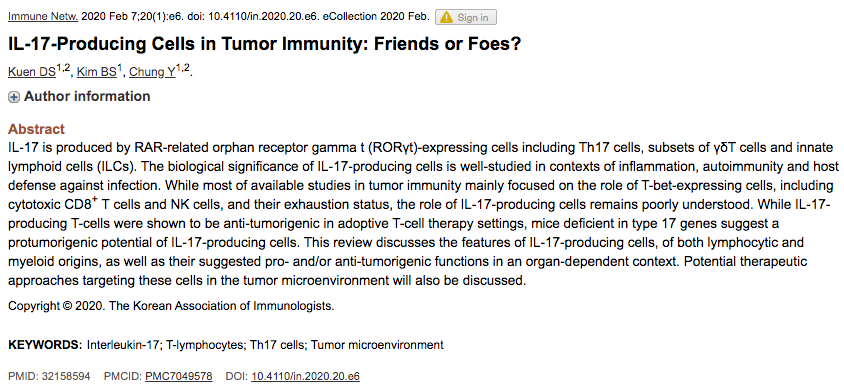
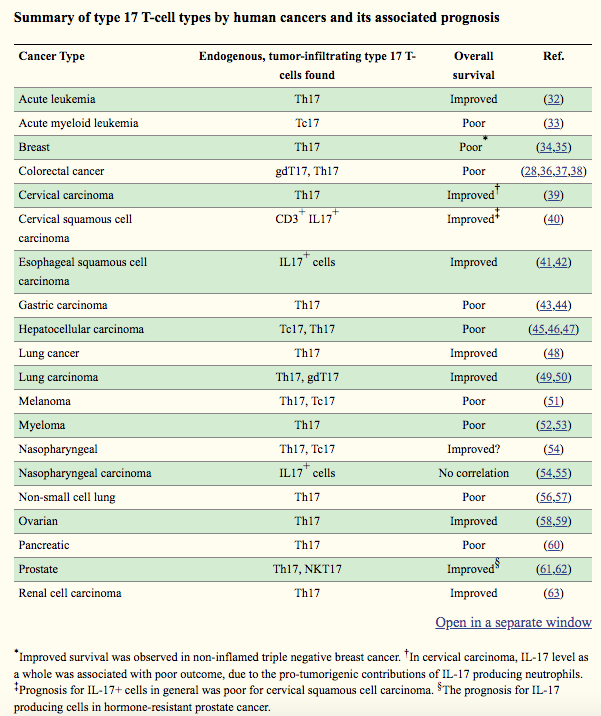
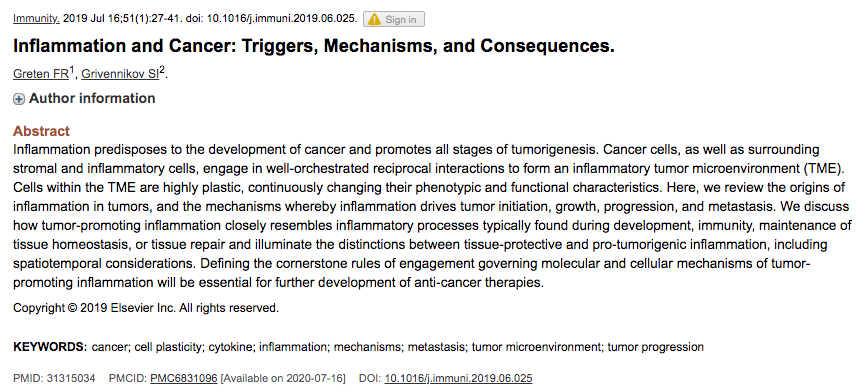
8)Cancers
IL-17A producing cells are closely associated w/cancer. Depending on cancer type, IL-17A may have pro or anti-tumorigenic effects.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7049578/
Chronic inflammation contributes to cancer development, growth, therapy resistance & metastasis (31315034)
8)Cancers
IL-17A producing cells are closely associated w/cancer. Depending on cancer type, IL-17A may have pro or anti-tumorigenic effects.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7049578/
Chronic inflammation contributes to cancer development, growth, therapy resistance & metastasis (31315034)
12/
9)BMI>40
see 2-11. Obesity/metabolic syndrome increases chances of all of these conditions.
9)BMI>40
see 2-11. Obesity/metabolic syndrome increases chances of all of these conditions.
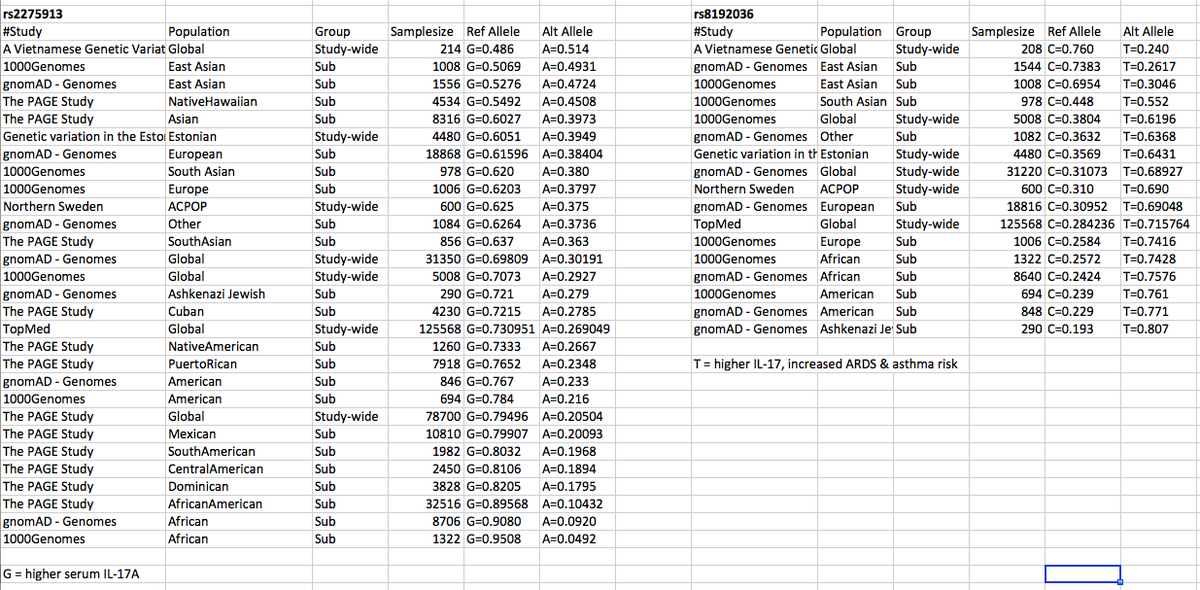
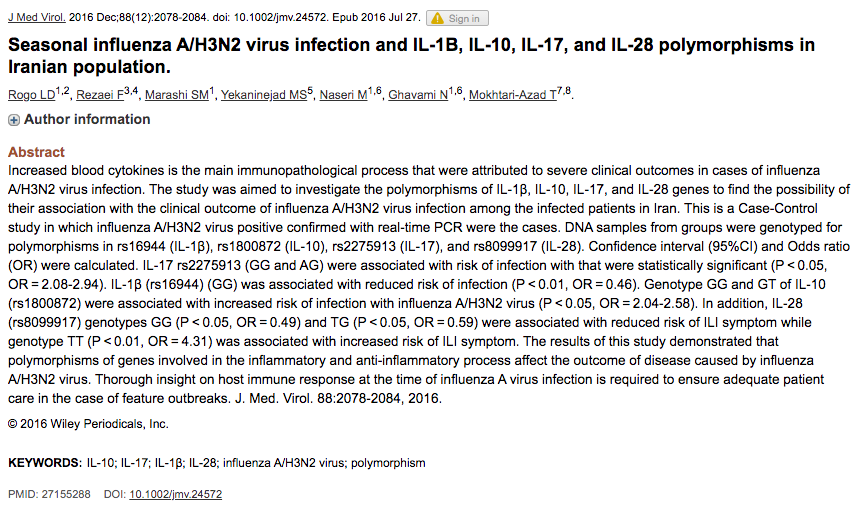
Couple IL-17A SNPs associated w/  susceptibility 2 ARDS, cerebrovascular disease, asthma, flu etc... May/may not be relevant 2 #covid19 . I lack expertise to critically evaluate GWAS lit, but putting here 4 someone else to investigate.
susceptibility 2 ARDS, cerebrovascular disease, asthma, flu etc... May/may not be relevant 2 #covid19 . I lack expertise to critically evaluate GWAS lit, but putting here 4 someone else to investigate.
 susceptibility 2 ARDS, cerebrovascular disease, asthma, flu etc... May/may not be relevant 2 #covid19 . I lack expertise to critically evaluate GWAS lit, but putting here 4 someone else to investigate.
susceptibility 2 ARDS, cerebrovascular disease, asthma, flu etc... May/may not be relevant 2 #covid19 . I lack expertise to critically evaluate GWAS lit, but putting here 4 someone else to investigate.
http://snpedia.com/index.php/Rs2275913
Metasite very useful for summarizing/aggregating references on polymorphisms.
If you did @23andMe sequencing, you can see pull your own data through these links:
https://geneticlifehacks.com/increased-inflammation-and-il-17a-polymorphisms/
https://www.geneticlifehacks.com/are-you-genetically-unlikely-to-get-the-flu/
Metasite very useful for summarizing/aggregating references on polymorphisms.
If you did @23andMe sequencing, you can see pull your own data through these links:
https://geneticlifehacks.com/increased-inflammation-and-il-17a-polymorphisms/
https://www.geneticlifehacks.com/are-you-genetically-unlikely-to-get-the-flu/
15/
How might chronic inflammation (& elevated IL-17A) contribute to #covid19 1) susceptibility and/or 2) severity?
IL-17A inhibits IFN-λ , the first line of defense against respiratory viruses! https://twitter.com/JukeBaRosh/status/1246917212549648391?s=20
How might chronic inflammation (& elevated IL-17A) contribute to #covid19 1) susceptibility and/or 2) severity?
IL-17A inhibits IFN-λ , the first line of defense against respiratory viruses! https://twitter.com/JukeBaRosh/status/1246917212549648391?s=20
17/
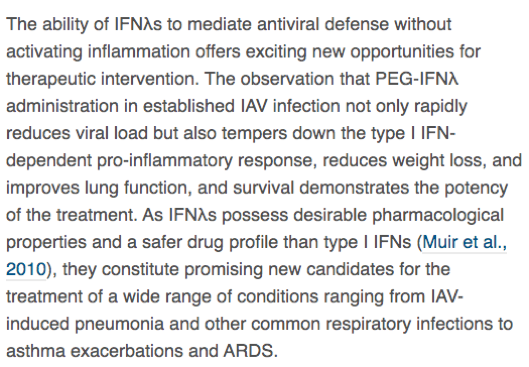
"•IFNλs are the 1st IFNs produced that suppress initial viral spread
•IFNλs exhibit potent antiviral functions w/o activating inflammation
•Type I IFNs come up later to enhance antiviral & pro-inflammatory responses"
https://doi.org/10.1016/j.immuni.2017.04.025
"•IFNλs are the 1st IFNs produced that suppress initial viral spread
•IFNλs exhibit potent antiviral functions w/o activating inflammation
•Type I IFNs come up later to enhance antiviral & pro-inflammatory responses"
https://doi.org/10.1016/j.immuni.2017.04.025
18/
This leads to 1st hypothesis:
Individuals w/inflammation that affects the airways (including the vasculature) are less able to activate an effective first line defense against CoV-2. This would mean that more virus can get past upper airway & into alveolar spaces of lungs.
This leads to 1st hypothesis:
Individuals w/inflammation that affects the airways (including the vasculature) are less able to activate an effective first line defense against CoV-2. This would mean that more virus can get past upper airway & into alveolar spaces of lungs.
19/
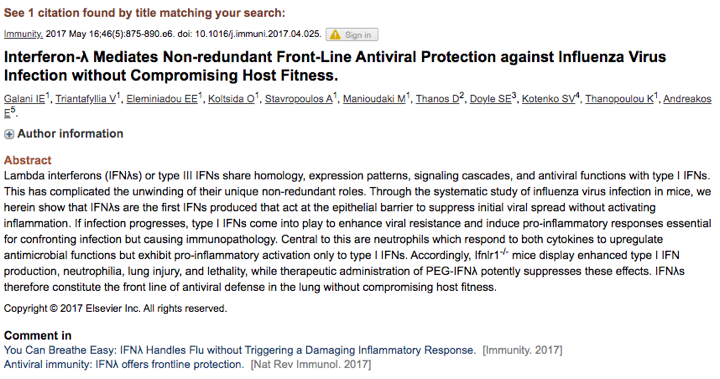
VIRAL LOAD appears 2 CORRELATE w/DISEASE severity (32199493). Severe patients in 1 study avg ~60X higher viral loads than mild cases. IF disease severity also correlates w/exposure load, then HEALTHCARE WORKERS ARE ESPECIALLY VULNERABLE. We're already seeing evidence of that.
VIRAL LOAD appears 2 CORRELATE w/DISEASE severity (32199493). Severe patients in 1 study avg ~60X higher viral loads than mild cases. IF disease severity also correlates w/exposure load, then HEALTHCARE WORKERS ARE ESPECIALLY VULNERABLE. We're already seeing evidence of that.
20/
Why might viral load lead to more severe disease?
#covid19 makes ORF1ab, a protein shown in SARS to halt/delay interferon (IFN) response, including IFN-λ.
(25481026/19369340/32270184)
DOI: 10.1016/j.cell.2020.04.026/. https://twitter.com/virusninja/status/1251171482463600640?s=20
Why might viral load lead to more severe disease?
#covid19 makes ORF1ab, a protein shown in SARS to halt/delay interferon (IFN) response, including IFN-λ.
(25481026/19369340/32270184)
DOI: 10.1016/j.cell.2020.04.026/. https://twitter.com/virusninja/status/1251171482463600640?s=20
21/
w/o IFNs, virus replicates longer & more macrophages/ neutrophils are recruited to infection.
w/o IFN-λ, immune cells responding to infection polarize as inflammatory, leading to pneumonia.
More virus, more inflammation, more severe disease http://ncbi.nlm.nih.gov/pmc/articles/PMC5701513/
w/o IFNs, virus replicates longer & more macrophages/ neutrophils are recruited to infection.
w/o IFN-λ, immune cells responding to infection polarize as inflammatory, leading to pneumonia.
More virus, more inflammation, more severe disease http://ncbi.nlm.nih.gov/pmc/articles/PMC5701513/
22/
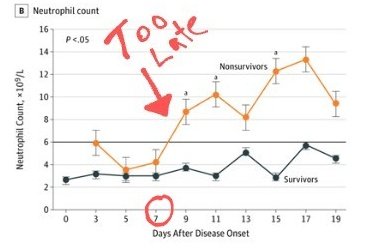
7-10 days post-symptom, severe cases either start getting better or their condition nose-dives, leading to acute respiratory distress syndrome, associated sepsis, & in ~40-70% of cases, death.
Timing of nosedive correlates with a number of markers.
7-10 days post-symptom, severe cases either start getting better or their condition nose-dives, leading to acute respiratory distress syndrome, associated sepsis, & in ~40-70% of cases, death.
Timing of nosedive correlates with a number of markers.
23/
A few:
Seroconversion (robust antibody response against virus)
https://twitter.com/JukeBaRosh/status/1245350460069941250?s=20
Increase in neutrophil count
https://twitter.com/JukeBaRosh/status/1244442983241564160?s=20
Increasing C-Reactive-Protein/lymphopenia
https://pubmed.ncbi.nlm.nih.gov/32259132/
A few:
Seroconversion (robust antibody response against virus)
https://twitter.com/JukeBaRosh/status/1245350460069941250?s=20
Increase in neutrophil count
https://twitter.com/JukeBaRosh/status/1244442983241564160?s=20
Increasing C-Reactive-Protein/lymphopenia
https://pubmed.ncbi.nlm.nih.gov/32259132/
24/
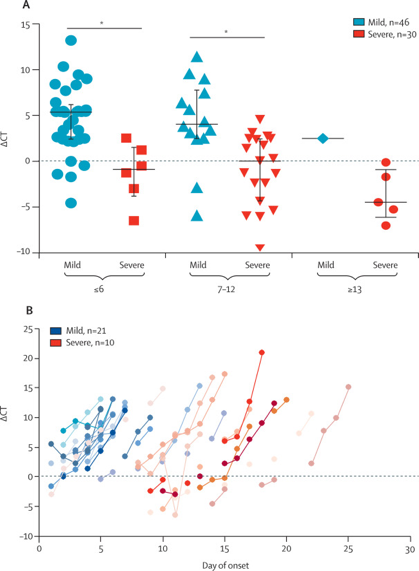
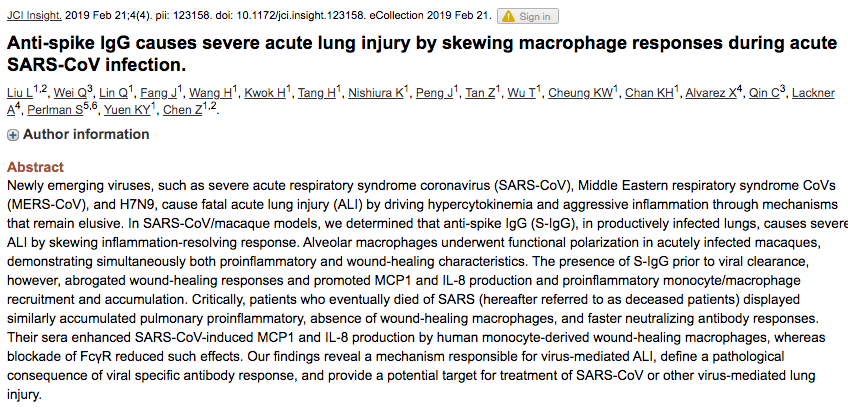
Seroconversion leads to complement activation.
ie: antibody binds virus & destroys.
Sounds like good thing, but if there's already massive inflammation (and limited ways to shut down) it's BAD.
w/ SARS, seroconversion was associated w/ ARDS/death.
https://twitter.com/JukeBaRosh/status/1245354391936401408?s=20
Seroconversion leads to complement activation.
ie: antibody binds virus & destroys.
Sounds like good thing, but if there's already massive inflammation (and limited ways to shut down) it's BAD.
w/ SARS, seroconversion was associated w/ ARDS/death.
https://twitter.com/JukeBaRosh/status/1245354391936401408?s=20
25/
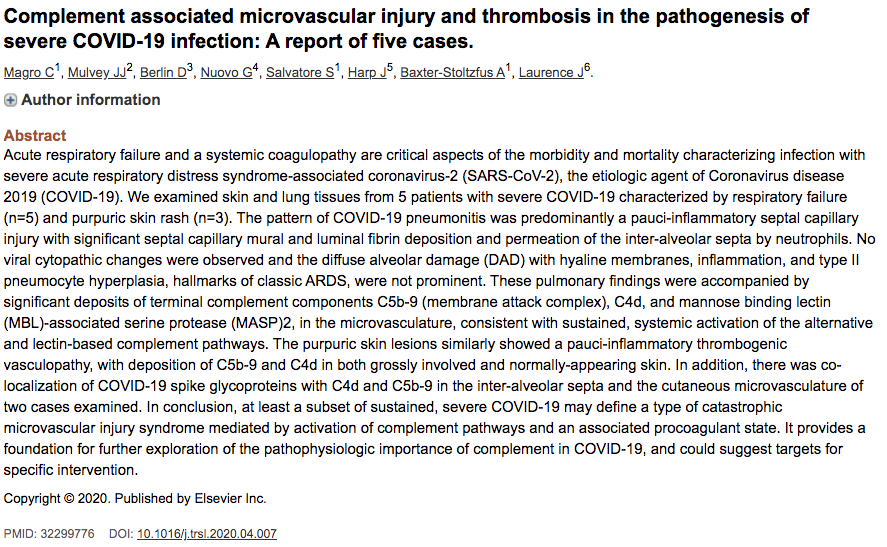
Complement activation has also been associated w/ severe cases of #covid19
"Our studies suggest that at least a subset of severe COVID-19 infection involves a catastrophic, complement-mediated thrombotic microvascular injury syndrome..."
DOI: 10.1016/j.trsl.2020.04.007
Complement activation has also been associated w/ severe cases of #covid19
"Our studies suggest that at least a subset of severe COVID-19 infection involves a catastrophic, complement-mediated thrombotic microvascular injury syndrome..."
DOI: 10.1016/j.trsl.2020.04.007
26/
Distancing can reduce, but not viral spread, & even PPE has limitations, so we need therapeutics
viral spread, & even PPE has limitations, so we need therapeutics
Ways to tackle:
1) inflammation
inflammation
2) front-line defenses in respiratory tract (esp upper)
front-line defenses in respiratory tract (esp upper)
3) target viral replication
4) target cytokine responses (& maybe complementation)
Distancing can reduce, but not
 viral spread, & even PPE has limitations, so we need therapeutics
viral spread, & even PPE has limitations, so we need therapeuticsWays to tackle:
1)
 inflammation
inflammation2)
 front-line defenses in respiratory tract (esp upper)
front-line defenses in respiratory tract (esp upper)3) target viral replication
4) target cytokine responses (& maybe complementation)
27/
Until there's ( ) vaccine, no way to stop virus. Chronic inflammation clearly puts people at higher risk.
) vaccine, no way to stop virus. Chronic inflammation clearly puts people at higher risk.
Many ways to inflammation
inflammation
 ACE2/ACE1 ratio
ACE2/ACE1 ratio
 IL10/IL-17A ratio
IL10/IL-17A ratio
 HDL/LDL ratio
HDL/LDL ratio
 blood sugar
blood sugar
 pressure
pressure
 BMI
BMI
Sometimes inflammation can't be controlled.
Until there's (
 ) vaccine, no way to stop virus. Chronic inflammation clearly puts people at higher risk.
) vaccine, no way to stop virus. Chronic inflammation clearly puts people at higher risk.Many ways to
 inflammation
inflammation ACE2/ACE1 ratio
ACE2/ACE1 ratio IL10/IL-17A ratio
IL10/IL-17A ratio HDL/LDL ratio
HDL/LDL ratio blood sugar
blood sugar pressure
pressure BMI
BMISometimes inflammation can't be controlled.
28/
Prophylactic pegalated IFN-λ is promising opt for high risk groups. Excellent saftey record. Can be produced on large scale (in bacteria). Trials for mild cases ongoing.
http://med.stanford.edu/news/all-news/2020/05/covid-19-drug-for-outpatients-tested.html
https://clinicaltrials.gov/ct2/show/NCT04343976
Prophylactic pegalated IFN-λ is promising opt for high risk groups. Excellent saftey record. Can be produced on large scale (in bacteria). Trials for mild cases ongoing.
http://med.stanford.edu/news/all-news/2020/05/covid-19-drug-for-outpatients-tested.html
https://clinicaltrials.gov/ct2/show/NCT04343976
29/
Some people will still get sick.
w/other viruses that replicate in Type II pneumocytes (eg. Influenza A strains) the amt of virus that reaches these cells matters.
In macaques, H5N1 trachea = mild disease, but same titer inhaled = ARDS/death. https://www.jimmunol.org/content/198/4/1616.long
trachea = mild disease, but same titer inhaled = ARDS/death. https://www.jimmunol.org/content/198/4/1616.long
Some people will still get sick.
w/other viruses that replicate in Type II pneumocytes (eg. Influenza A strains) the amt of virus that reaches these cells matters.
In macaques, H5N1
 trachea = mild disease, but same titer inhaled = ARDS/death. https://www.jimmunol.org/content/198/4/1616.long
trachea = mild disease, but same titer inhaled = ARDS/death. https://www.jimmunol.org/content/198/4/1616.long
30/
So what about people that get sick? Trials ongoing for many drugs.
8+ days post-symptom, when infectious virus can't be recovered, is likely 2 late to give drugs targeting viral entry & replication.
Prophylactic/early onset trials are needed to assess efficacy.
32031570
So what about people that get sick? Trials ongoing for many drugs.
8+ days post-symptom, when infectious virus can't be recovered, is likely 2 late to give drugs targeting viral entry & replication.
Prophylactic/early onset trials are needed to assess efficacy.
32031570
31/
Pathology is driven not by virus itself, but an uncontrolled hyperinflammatory response that occurs ~ the time of seroconversion (avg 7-10 days). https://www.nature.com/articles/s41577-020-0331-4?utm_source=facebook&utm_medium=social&utm_content=organic&utm_campaign=NGMT_USG_JC01_GL_NRJournals
Pathology is driven not by virus itself, but an uncontrolled hyperinflammatory response that occurs ~ the time of seroconversion (avg 7-10 days). https://www.nature.com/articles/s41577-020-0331-4?utm_source=facebook&utm_medium=social&utm_content=organic&utm_campaign=NGMT_USG_JC01_GL_NRJournals
32/
Neutrophilic inflammation causes tissue damage, fluid accumulayion, & NETS; neutrophil counts in serum r associated w/morbidity.
neutrophil counts in serum r associated w/morbidity.
Therapeutics given early, 2 neutrophil accumulation, are logical drug candidates.
neutrophil accumulation, are logical drug candidates.
IL-17A is one such candidate https://twitter.com/NatRevImmunol/status/1257344861021364227?s=19
Neutrophilic inflammation causes tissue damage, fluid accumulayion, & NETS;
 neutrophil counts in serum r associated w/morbidity.
neutrophil counts in serum r associated w/morbidity.Therapeutics given early, 2
 neutrophil accumulation, are logical drug candidates.
neutrophil accumulation, are logical drug candidates.IL-17A is one such candidate https://twitter.com/NatRevImmunol/status/1257344861021364227?s=19
33/
Another potential benefit of targeting IL-17A is that it completely reverses the steroid insensitivity of neutrophilic inflammation #inmice. This paper is from Feb 2020.
https://insight.jci.org/articles/view/132836
Another potential benefit of targeting IL-17A is that it completely reverses the steroid insensitivity of neutrophilic inflammation #inmice. This paper is from Feb 2020.
https://insight.jci.org/articles/view/132836
34/
At every stage, there's good case 4 testing IL-17A inhibitors
1) prophylactically ( IFN-λ)
IFN-λ)
2) early ( neutrophil)
neutrophil)
3) late (possibly steroid resistance)
steroid resistance)
Moreover, there R already FDA approved α-IL-17A Abs & a small molecule inhibitor, cyanidin. https://pubmed.ncbi.nlm.nih.gov/28223414/
At every stage, there's good case 4 testing IL-17A inhibitors
1) prophylactically (
 IFN-λ)
IFN-λ)2) early (
 neutrophil)
neutrophil)3) late (possibly
 steroid resistance)
steroid resistance)Moreover, there R already FDA approved α-IL-17A Abs & a small molecule inhibitor, cyanidin. https://pubmed.ncbi.nlm.nih.gov/28223414/

 Read on Twitter
Read on Twitter