People who are dying of COVID19 will need first-rate palliative (hospice) care. This is going to be especially the case for people who are denied ventilators or who are taken off of them (i.e., who are “extubated”). Let’s talk about this painful and poignant fact. 1/
It’s not just a question of “optimal” triage polices for access to ventilators or ICU beds (now tragically being promulgated in hospitals around the USA). Rather, it's a question regarding how will we care for the COVID19 patients whom we triage to allow to die. 2/
Especially if we resort to battlefield triage as in Italy, we will need to plan for palliative care. This will involve drugs to relieve pain, dyspnea, anxiety, and other symptoms near death. This means we need opioids and benzodiazepines (e.g., morphine and midazolam). 3/
I was a practicing hospice doctor from 1995 to 2010. I was able, as a result of this privileged opportunity, to observe very many people near death, and to do my best to help them. I practiced at @HorizonHospice & @UChicago and later at @MassGeneralNews & @MountAuburnHosp 4/
I am very worried we will not have the medications (and personnel) we need in the USA to properly treat symptoms of dyspnea (shortness of breath), air hunger, pain, thirst, and anxiety near the end of life for COVID19 patients denied ventilators. @NHPCO_news 5/
And I am worried we are not adequately prepared to cope with the psychological aspects of often unusual COVID19 deaths (sudden, alone, or as a result of triage, etc.) either — for the patients themselves (if they are conscious) and their families. 6/
We need to plan now for this, as I noted on March 22: https://twitter.com/NAChristakis/status/1241864708744937472?s=20 7/
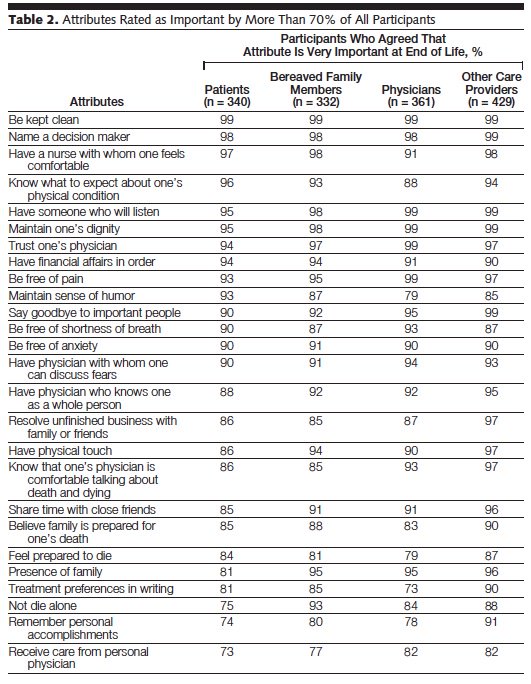
There is wide agreement among patients, families, and doctors in the USA about what is important at the end of life. http://jamanetwork.com/journals/jama/fullarticle/193279 Unsurprisingly, 93% of Americans feel that being free of pain and other symptoms (such as dyspnea) is “very important.” 8/
Dyspnea and air hunger at the end of life are truly awful. These symptoms are often worse than pain, and often harder to treat. Like other hospice doctors (and nurses), I have seen this up close. 9/
Also important to patients: 81% of Americans rate having family present at death as “very important” when they die. The great majority of people do not wish to die alone. http://jamanetwork.com/journals/jama/fullarticle/193279 10/
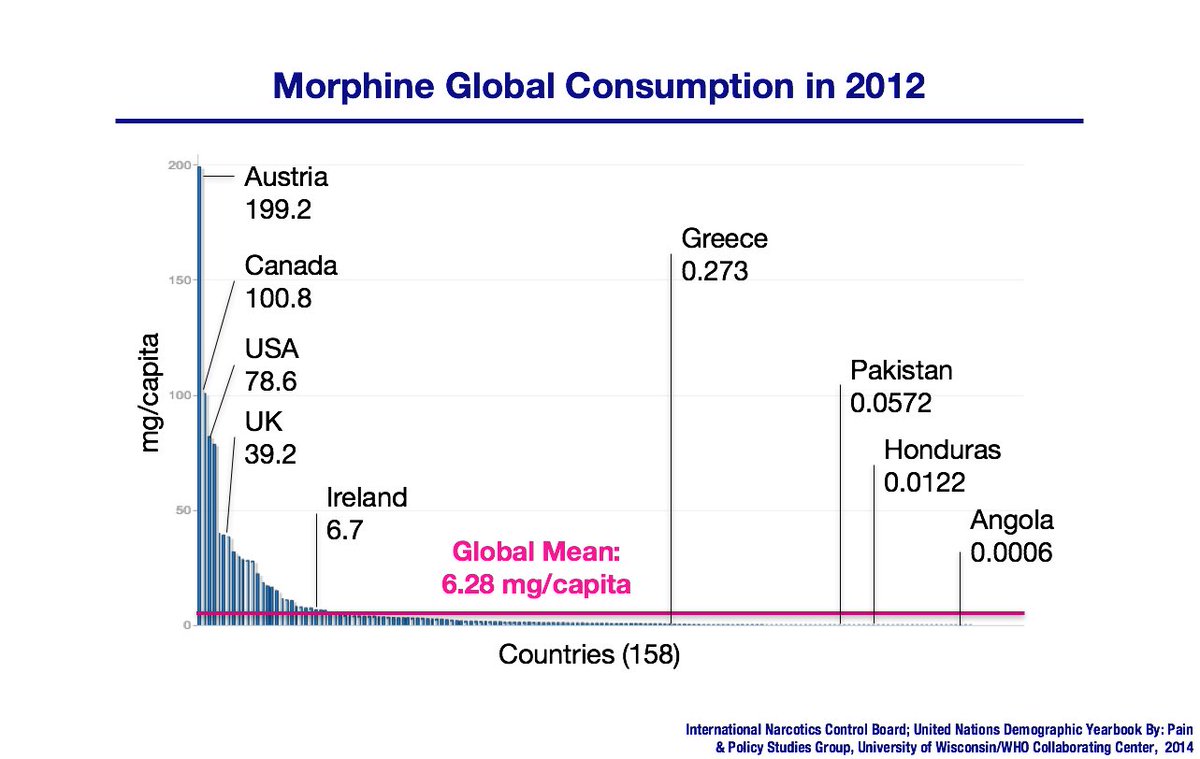
The use of opioids in medical care is high in the USA compared to most other countries, at baseline, for a variety of reasons, including our wealth. 11/
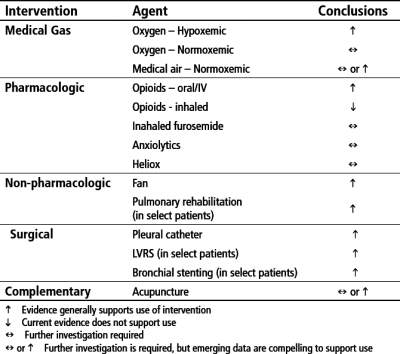
Opioids (e.g., morphine, fentanyl) are the mainstay of treatment for dyspnea, though benzodiazepines which relieve anxiety (e.g., valium, midazolam) help a lot. And there are other tricks that sometimes help (like inhaled furosemide). 12/
Positioning of patients on their bellies or sides can help with air hunger, but only a bit, if we are really talking about extubating critically ill patients to free up ventilators. Such patients are extremely sick. They require expert palliative care. 13/
Death is not immediate after disconnection from a ventilator (extubation). For instance, in one study of 12 patients in a community hospital in Taiwan, death ensued from 20 minutes to 97 hours after extubation. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4396346/ 14/
Here is a nice review regarding treating dyspnea at the end of life, e.g., in extubated patients: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3304253/ The pharmacological tools at our disposal are powerful, if limited. 15/
Where do we stand in terms of our preparation to care for COVID19 patients, not just in terms of beds and palliative medicine personnel, but also the crucial drugs for treating such patients, if they have been triaged away from ventilators? 16/
In many cases, the sedative and other drugs needed to treat COVID19 patients triaged to not get ventilators are the same as those necessary to care for patients on ventilators! 17/
There has been a 51% increase in demand already in March in the USA for various sedatives and anesthetics: propofol, dexmedetomidine, etomidate, ketamine, lorazepam, and midazolam. https://www.statnews.com/pharmalot/2020/03/31/a-new-covid-19-problem-shortages-of-medicines-needed-for-placing-patients-on-ventilators/ 18/
Similarly, the demand for three analgesics — hydromorphone, fentanyl, and morphine — rose 67% so far in March in the USA. https://www.statnews.com/pharmalot/2020/03/31/a-new-covid-19-problem-shortages-of-medicines-needed-for-placing-patients-on-ventilators/ 19/
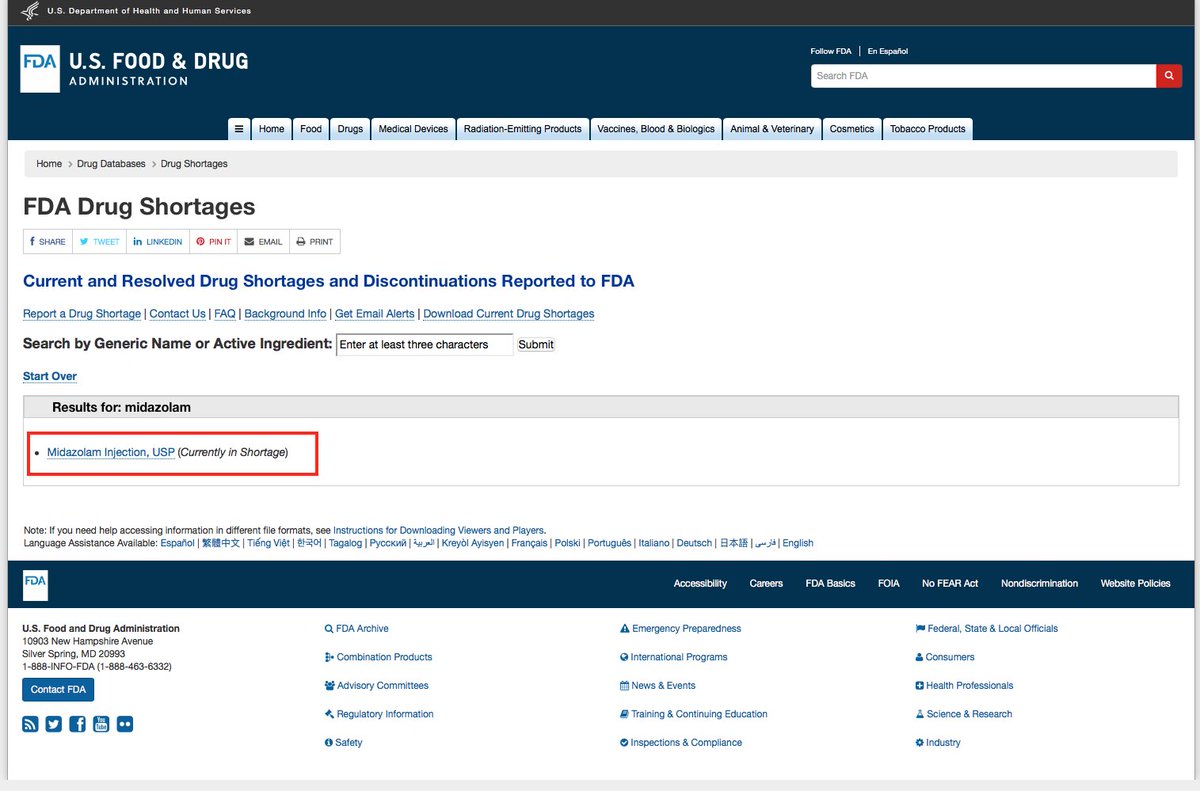
You can use this @US_FDA website to check which drugs are “currently in shortage." https://www.accessdata.fda.gov/scripts/drugshortages/ 20/
And midazolam is already in shortage! It’s hard to emphasize how important a drug it is, both for treating ICU patients and for palliative care — though, in palliative care, we could switch to longer-acting agents, like valium, which would relieve shortage for ICU patients. 21/
Using such drugs to palliate symptoms in patients taken off ventilators might accelerate death, some will say. But what is the alternative, since, without a ventilator, the patients are slated to die anyway? Shall we let them suffer? 22/
Of course, we also need these agents to actually treat patients with COVID19 who are *not* expected to die! These drugs are essential to keep patients sedated while they are on a ventilator. Otherwise, they often thrash and pull out their life-saving tubes. 23/
But the drug supply chain is one of just-in-time production and distribution. Nobody has 2 times, let alone 10 times, the amount of drugs on hand that are going to be needed for the surge in COVID19 patients. We need more drugs now. 24/
The supply chain for many drugs goes through India and China, and this pandemic has highlighted how, when catastrophe strikes, each country looks to its own needs. This is not just with respect to PPE or ventilators, but basic and crucial drugs. [thread continues...] 25/
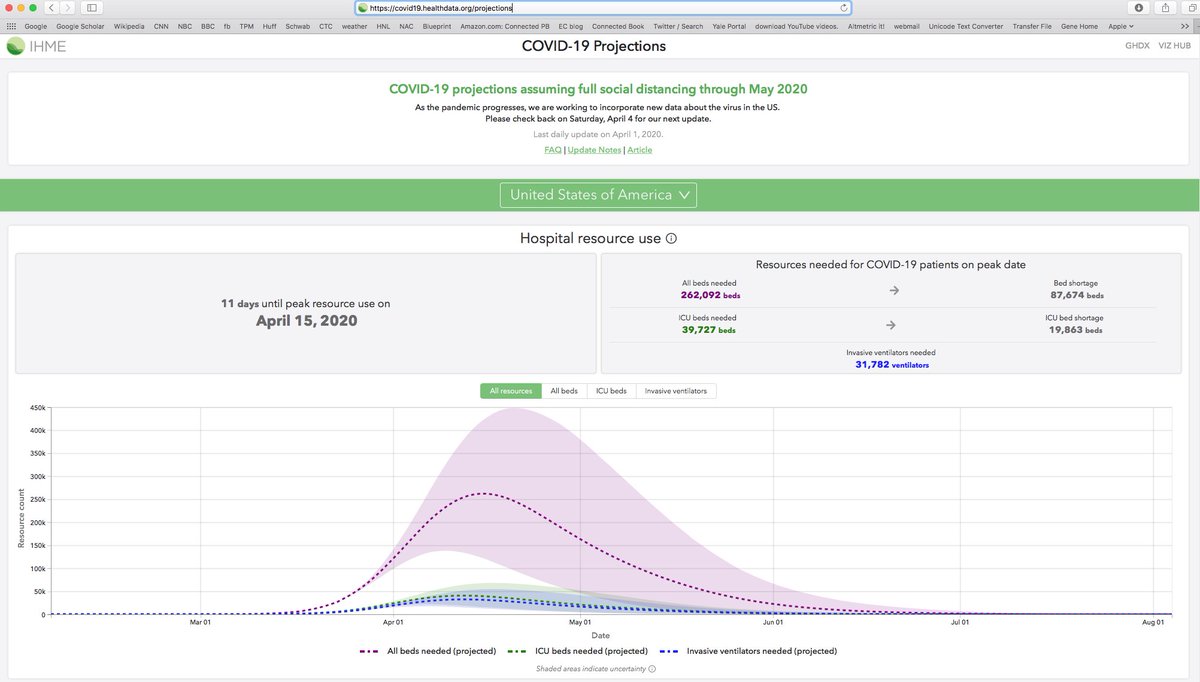
We will have many thousands of people in this predicament. In the USA as a whole, we are estimated to reach peak resource demands for COVID19 patients on April 15. We will need 31,782 ventilators, and we are short. https://covid19.healthdata.org/projections 26/
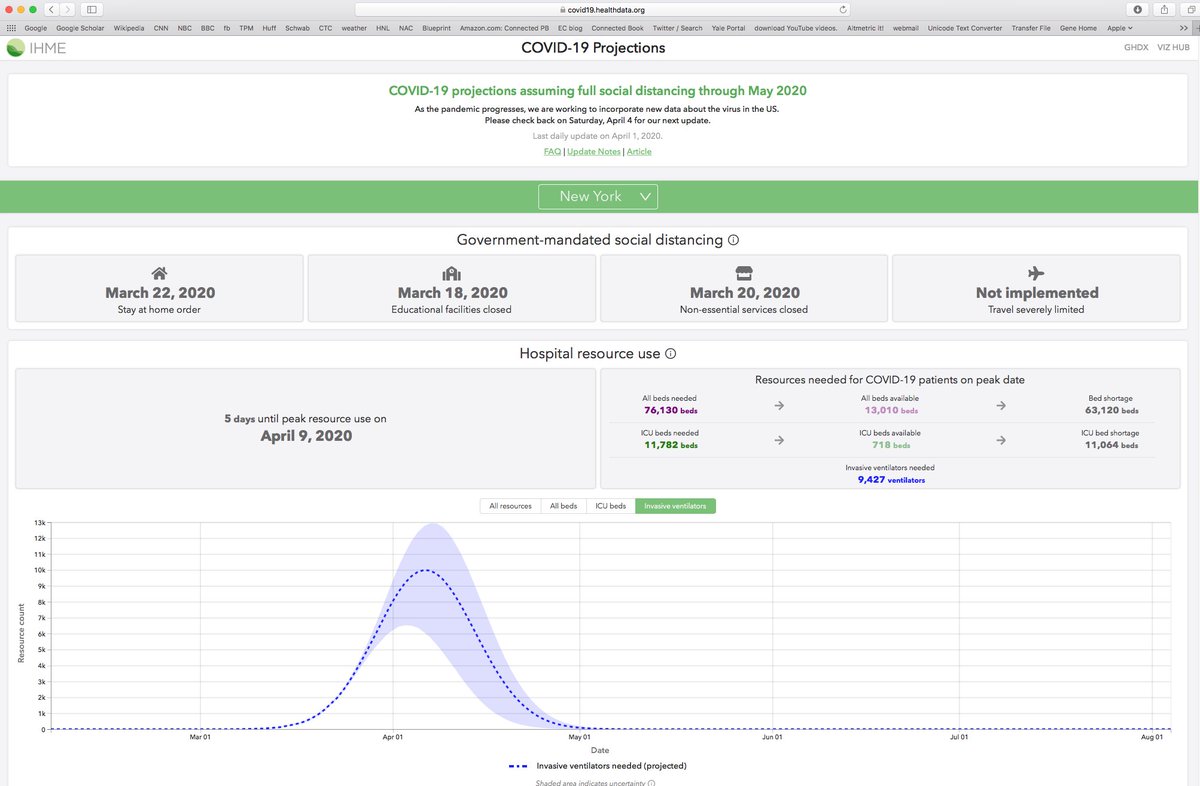
In New York state (as of today, April 4), we are 5 days from peak demand. Yet we estimate a rough shortfall of 11,064 ICU beds and 9,427 ventilators. That is a lot of patients who will be triaged away from ventilators and who will need palliative care! https://covid19.healthdata.org/projections 27/
As a hospice doctor, I used to say: “While we cannot stop your disease, there is much that we can do to care for you. And I promise I will not abandon you.” But how can we provide care without basic medicines? 28/
Dying alone is also awful. This can happen to COVID19 patients for a number of reasons, including hospital policies related to reducing transmission to family members (given the lack of PPE to spare for them) and the frequent suddenness of death in this condition. 29/
In the case of COVID19, stories are emerging of people saying goodbye via video link, and dying alone! As a hospice doctor, this makes me weep. https://www.cnn.com/2020/03/29/world/funerals-dying-alone-coronavirus/index.html 30/
All of this will be so much worse in the poor countries of the world. There, people will die without any medical care at all, as they do even in the best of times. But just look at poor Ecuador facing COVID19 now: https://www.cnn.com/2020/04/03/americas/guayaquil-ecuador-overwhelmed-coronavirus-intl/index.html 31/
Home hospice care for non-COVID19 patients is also being affected by the COVID19 crisis. The lack of PPE is making things hard. Here are two examples, in Idaho and Texas: https://idahonews.com/news/coronavirus/treasure-valley-hospice-providing-care-in-the-face-of-covid-19 & https://twitter.com/CommHealthTX/status/1246113426168053760?s=20 32/
Providing good hospice care is not as technically demanding as providing good ICU care, but we will likely have a shortfall of experienced practitioners here too, just as with ICU care. 33/
We have to accept that death will haunt our streets during this plague, and that there will be many deaths. 34/
But for the deaths we cannot prevent, either arising from directly from COVID19 itself or from our lack of personnel or equipment, we must prepare to provide for humane deaths, unless we truly want the streets of the USA to be awful killing fields. 35/
Fine essay by @zeynep in @TheAtlantic on the problem, noted earlier, of dying alone during pandemics, which has been observed since ancient time. The dying are abandoned. As a hospice doctor, this is appalling, and unnecessary. https://www.theatlantic.com/health/archive/2020/07/covid-dying-words/613951/ 36/
If true, this should offend our conscience. Dying alone, with loved ones visiting via iPad, is unnecessary: if we had done a better job with this second wave to reduce the number of deaths & hospital congestion, we would not be in this APALLING place. https://twitter.com/roto_tudor/status/1334534101265682434?s=20 37/

 Read on Twitter
Read on Twitter